Low Libido in Men: Signs, Causes, and Next Steps—A Clinical and Psychological Overview
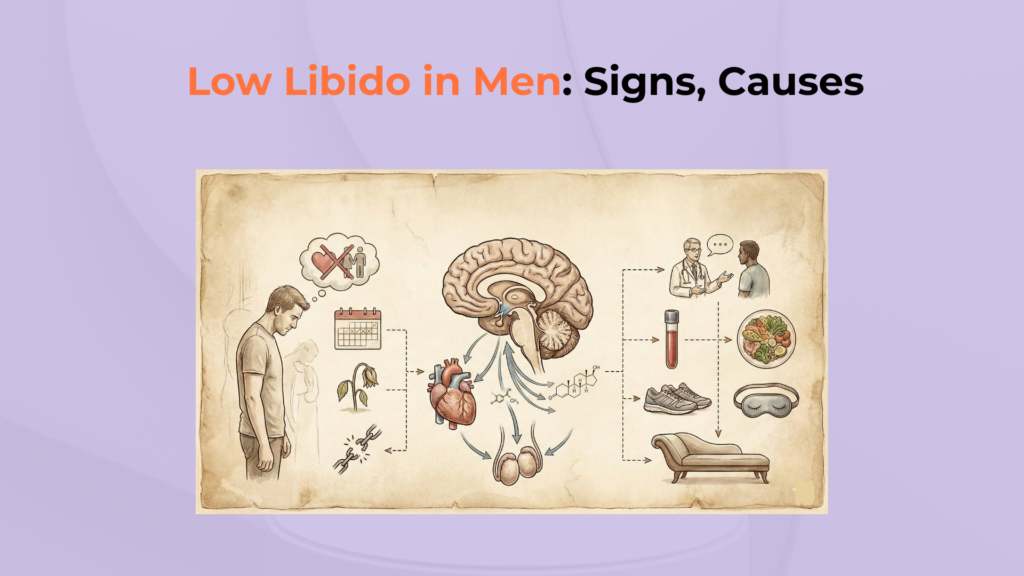
Low libido in men—often described clinically as low sexual desire or Male Hypoactive Sexual Desire Disorder (MHSDD)—involves a persistent reduction in sexual thoughts and desire that may cause personal distress or relationship difficulty [LL1, LL8].
It is a biopsychosocial condition distinct from Erectile Dysfunction, involving hormonal, psychological, and systemic pathways.
If you want the clean baseline definition of “libido” (desire) before troubleshooting, start with Male Libido, because many men are actually describing performance problems—not desire loss.
If this feels like a change from your normal pattern, use Libido Variability in Men to separate normal fluctuation from a clinically meaningful drop—and if it was abrupt, jump straight to Sudden Libido Drop in Men.
A significant drop in sexual desire can be an early marker for broader health issues, including testosterone deficiency (hypogonadism), metabolic disease, sleep disorders, medication effects, and depression [LL1] [LL6] [LL7].
Important Medical Disclaimer
This guide is for educational purposes only. Sudden or persistent loss of libido can indicate underlying conditions such as pituitary disorders, cardiovascular disease, sleep apnea, medication side effects, or depression. Consult a healthcare provider for a full evaluation.
Low Libido (Male HSDD): At a Glance
- What is it? Reduced “wanting/motivation,” distinct from erection mechanics.
- Key Causes Low Testosterone/Hypogonadism (Low T → Libido), medication effects (SSRIs, Finasteride), sleep disorders (Sleep Apnea), and mood/drive suppression (Depression).
- Diagnosis Requires structured assessment + morning labs.
- First Step Check Baseline (Hormones) + Lifestyle (Sleep/Stress).
What Is the Medical Definition of Low Libido?
Medically, problematic low libido is typically defined as persistently reduced sexual desire accompanied by clinically significant distress or interpersonal difficulty [LL1, LL8].
Defining Hypoactive Sexual Desire Disorder (HSDD)
Clinically, low libido aligns with Male Hypoactive Sexual Desire Disorder (MHSDD) when reduced sexual thoughts and desire are persistent (typically >6 months) and create marked distress [LL1, LL8].
It must be distinguished from Erectile Dysfunction (performance issue) and fertility problems. EAU Guidelines emphasize that lack of desire should be the principal complaint [LL1].
Persistent low desire creates distress or relationship impact, supporting a diagnosis of Male HSDD.
The Premise: Baseline vs. Sudden Drop
Identifying problematic low libido requires comparing your current desire to your personal baseline rather than to cultural stereotypes [LL1].
If your desire level has been consistently low for years without distress, it may simply reflect a stable baseline—see Stable Libido in Men. If your desire comes and goes, the correct frame is often fluctuation and triggers—see Fluctuating Libido in Men and Libido Tracking to identify the pattern before assuming “hormones.”
A naturally lower baseline can be normal if stable; a sudden drop often signals a change in health, meds, or mood [LL3] [LL5].
As noted by Levine, variability of sexual drive is high, but a significant drop from baseline signals an underlying shift in health that warrants structured medical review [LL1].
What Are the Primary Physical and Hormonal Causes of Low Libido?
For a structured map of male desire types and drivers, start with Male Sex Drive. Physical causes of low libido most often involve androgen deficiency evaluation, medication effects, sleep disorders, and cardiometabolic health [LL1] [LL2] [LL5] [LL9].
If you’re unsure whether you need “labs first” or “lifestyle first,” use Libido Assessment and Low Libido Labs (Men) so you don’t miss common reversible medical causes.
Hypogonadism (Low Testosterone)
Hypogonadism (testosterone deficiency) is a common reversible contributor because androgen signaling supports sexual desire pathways [LL1] [LL2].
AUA guidance uses total testosterone <300 ng/dL as a diagnostic cut-off, confirmed by repeat early morning testing [LL2].
Clinically, it helps to separate “total testosterone” vs “free testosterone” when symptoms and numbers don’t match—see Testosterone and Libido and Free Testosterone and Libido. If Low T is confirmed and symptomatic, the next step is evidence-based management—not guesswork—see Low Testosterone Treatment (Libido).
The Endocrine Society emphasizes that diagnosis requires both low levels and symptoms [LL4].
Confirmed low testosterone contributes to low libido, and clinician-guided therapy may improve desire in selected men.
If testosterone is borderline but libido is clearly low, clinicians often screen “blockers” like prolactin and thyroid dysfunction—see Prolactin and Libido, Hypothyroidism and Libido, and Hyperthyroidism and Libido.
Medication Side Effects (The Iatrogenic Cause)
Medication effects are a frequent iatrogenic driver of low libido, especially agents that shift serotonin/dopamine balance or alter androgen metabolism [LL3].
The highest-yield medication categories to audit are serotonergic antidepressants and androgen-modulating drugs: start with SSRIs and Libido, then broaden to Antidepressants and Libido. If a switch is being considered (clinician-led), see Bupropion and Libido and SSRI Management (Libido).
SSRIs are strongly associated with sexual side effects; Finasteride has documented associations in some men [LL3] [LL10] [LL11].
For drug-specific context and risk framing, see Finasteride and Libido. If you’re also on cardiometabolic meds, these can contribute in susceptible men—see Beta-Blockers and Libido and Statins and Libido.
Management strategies include dose adjustment or switching, as cited by Jing and Montejo [LL3]. Do not stop medications abruptly; discuss alternatives with your prescriber.
Lifestyle and Systemic Health
Lifestyle and systemic health factors—especially sleep apnea and metabolic syndrome—can suppress libido via endocrine disruption, inflammation, and vascular risk [LL5] [LL9].
Sleep is one of the most common “silent” drivers of libido suppression; if you have snoring/unrefreshing sleep, start with Sleep Apnea and Libido, and if the issue is simply short or fragmented sleep, see Sleep Deprivation and Libido and Insomnia and Libido.
Testosterone release is sleep-linked; Obstructive Sleep Apnea (OSA) is associated with lower testosterone [LL13].
Sleep restriction significantly reduces daytime testosterone levels [LL12] [LL5]. Sleep fragmentation reduces sleep-linked testosterone release, worsening libido and energy.
If low libido clusters with weight gain or metabolic markers, follow the cardiometabolic chain: Obesity, Diabetes, Hypertension, and Cardiovascular Health and Libido. If alcohol or cannabis are frequent, audit them here: Alcohol and Cannabis.
How Do Psychological and Emotional Factors Suppress Sexual Drive?
If you’re trying to determine whether the issue is “no spontaneous desire” versus “desire appears only after context,” compare Spontaneous Libido vs Responsive Libido. Psychological factors suppress libido by increasing inhibitory stress physiology, reducing reward sensitivity, and blunting pleasure (anhedonia) in depression [LL6] [LL7].
Chronic Stress and Cortisol
Chronic stress is associated with lower sexual arousal and can contribute to reduced libido through heightened inhibitory tone and attentional interference [LL6].
When desire shuts down under load, it’s often a stress-physiology problem rather than “attraction loss”—see Stress and Libido, Chronic Stress and Libido, and Cortisol and Libido.
Stress biology (including cortisol patterns) can impair sexual function, though individual responses vary. Hamilton notes the link between stress load and arousal inhibition [LL6].
Sustained stress load increases inhibition and reduces erotic attention, diminishing sexual desire.
Depression and Anhedonia
Depression often reduces libido via Anhedonia—the reduced ability to feel pleasure or motivation—which affects sexual interest directly [LL7].
Low libido can be both a symptom of the depression and a side effect of SSRI treatment [LL3].
If low desire is paired with low motivation, rumination, or dread around intimacy, route to the specific driver: Depression and Libido, Anxiety and Libido, or (when applicable) Grief and Libido and Burnout and Libido.
Calabrò highlights the neurobiology of sexual desire in mood disorders [LL7]. Treating the underlying mood disorder is frequently the first step toward restoring desire.
Comparison: Low Libido vs. Erectile Dysfunction (ED)
For a full comparison, see the Libido vs. Erectile Function guide. Low libido is primarily a reduction in desire (“mental wanting”), while erectile dysfunction is primarily a performance/physiologic erection issue—though they can co-occur [LL1].
If your symptoms feel more like “desire is present but the body doesn’t respond,” start with Erectile Dysfunction and Libido (and if both are low together, see ED + Low Libido in Men). If the confusion is “desire vs arousal,” the closest conceptual bridge is Libido vs Arousal in Men.
Diagnostic Differentiation Matrix
| Feature | Low Libido (Male HSDD) | Erectile Dysfunction (ED) |
|---|---|---|
| Primary Complaint | “I don’t feel interest/drive.” | “I want sex but can’t stay hard.” |
| Desire vs Performance | Desire-first problem. | Vascular/Neuro/Mechanical problem. |
| Morning Wood | May be reduced (androgen link); often preserved if psychogenic. | May be reduced in organic ED. |
| Common Drivers | Depression, SSRIs, Hypogonadism, Sleep Apnea. | Vascular disease, Diabetes, Meds, Nerves. |
| Typical First Steps | Biopsychosocial assessment + Labs. | Cardiometabolic risk eval + PDE5i. |
What Are the Next Steps for Diagnosing and Treating Low Libido?
Diagnosis and treatment require a structured biopsychosocial assessment, targeted labs, and cause-specific interventions (sleep, meds, therapy, hormones) [LL1, LL4].
Step 1: Comprehensive Blood Work
Start with a biopsychosocial assessment and order early-morning fasting Total Testosterone (repeat if low), adding Free Testosterone, Prolactin, and Thyroid testing when indicated [LL2, LL4].
If you want the exact ordering logic and why timing matters, see Testosterone Testing for Libido and the complete panel guide in Low Libido Labs (Men).
Endocrine Society emphasizes accurate assays and repeat morning testing before diagnosis [LL4].
The AUA testing protocol provides the standard for evaluation [LL2]. This helps rule in/out hypogonadism and hyperprolactinemia.
Step 2: Lifestyle Intervention
Lifestyle intervention targets high-yield drivers: sleep quality, weight, insulin resistance, alcohol, and activity [LL5] [LL9].
Screen for Sleep Apnea if snoring or unrefreshing sleep is present, as treatment can improve sexual health [LL13].
Schulster notes the strong link between metabolic syndrome and sexual dysfunction [LL9]. These steps create the physiologic conditions for libido to return.
If you want a step-by-step protocol rather than generic advice, use Libido Improvement (Men) plus the two highest yield levers: Sleep Restoration and Stress Management.
Step 3: Psychological or Relationship Counseling
Psychological or relationship counseling can reduce performance anxiety (“spectatoring”), improve erotic communication, and break avoidance loops [LL1].
If the drop tracks conflict, disconnection, or desire discrepancy, route here first: Relationship Stress and Libido. If the core issue is mood, pair therapy with evidence-based treatment routing: Depression Treatment and Libido.
EAU Guidelines emphasize addressing relationship factors as part of management [LL1].
This remains valuable even when physical causes exist, because desire is biopsychosocial. Examples include stress management and desire discrepancy work.
[Checklist] Auditing Your Symptoms for Low Libido
Use this checklist to track symptoms and prepare for a conversation with your healthcare provider.
Functional and Health Audit
- Duration: Has reduced interest persisted and caused distress? (Male HSDD criteria) [LL1, LL8].
- Baseline Shift: Sudden change after stress, illness, or life event? [LL1]. Low Libido Warning Signs and Sudden Libido Drop
- Morning Labs: Have you had repeat early-morning testosterone? [LL2, LL4]. Testosterone Testing
- Medications: Taking SSRIs, Finasteride, or BP meds? [LL3, LL10]. SSRIs, Finasteride, Beta-Blockers
- Sleep: Snoring or unrefreshed? (Screen for Apnea) [LL13]. Sleep Apnea
- Metabolic: Waistline, BP, Glucose check? (Metabolic Syndrome) [LL9].
- Mood: Anhedonia or low motivation? (Depression screen) [LL7]. Depression and Anxiety
- Safety Rule: Persistent low libido can reflect systemic disease; don’t ignore cardiometabolic risks [LL1, LL9].