Male Libido vs. Arousal: Key Differences Explained—Analyzing Desire vs. Physical Response
Understanding why the “mind” (Libido) and “body” (Arousal) don’t always agree.
Listen to Article
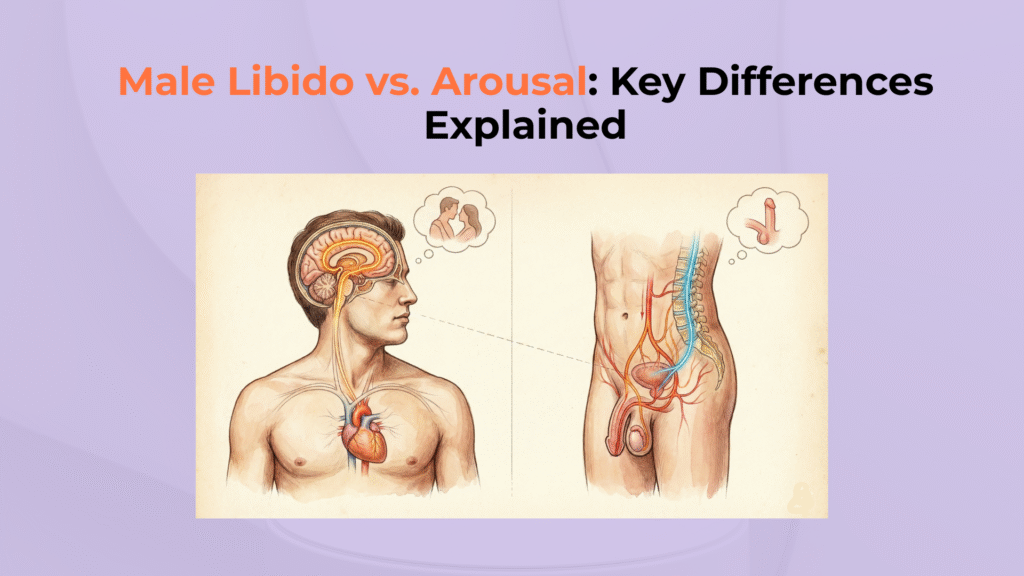
The distinction between Male Libido and Arousal lies in the separation of the “mental appetite” for sex (Libido) from the “physical reaction” of the genitalia (Arousal) [LA1].
If you’re new to the terminology, anchor the baseline first: in our Libido Hub, we define libido as a motivational “wanting” state rather than a reflex—see Male Sex Drive (clinical definition + desire types), then come back here to separate desire from erection mechanics.
While often used interchangeably in casual conversation, these are distinct biological systems: Libido is a dopaminergic and hormonal motivation state, whereas Arousal is a vascular and autonomic response [LA2].
Libido is fundamentally a reward-and-hormone problem: when dopamine incentive salience is low, the brain may not tag sex as “worth pursuing,” even if the body can still respond—our deep dive on Dopamine and Libido explains this “wanting vs. liking” mismatch.
Knowing which system is failing determines which fixes are realistic—whether focusing on hormonal balance (Testosterone optimization) or vascular health (Erectile Function mechanics).
Testosterone is best understood as a permissive threshold for desire circuits (not a simple volume knob), which is why some men have erections but low drive—see Testosterone and Libido in Men (threshold model).
A failure in libido requires a metabolic or psychological approach, while a failure in arousal often demands cardiovascular or neurological intervention involving the Parasympathetic Nervous System.
Important Medical Disclaimer
This guide is for educational purposes only. Persistent discordance between desire and physical function can indicate specific medical conditions ranging from Hypogonadism to Cardiovascular Disease. Consult a physician for diagnosis.
Libido vs. Arousal: At a Glance
- Driven by Testosterone & Dopamine.
- Mental motivation & appetite.
- Key Check: If you have erections but no desire, it’s a Libido issue.
- Driven by Blood Flow & Nerves.
- Physical vascular engorgement.
- Key Check: If you have desire but no erection, it’s an Arousal issue.
Where this topic fits in the Libido Hub
This guide separates the motivation system (libido) from the hardware system (erection mechanics) so you can target the right fix instead of guessing.
- Start here (definitions): If you want the complete framework for male desire—including spontaneous vs. responsive patterns—read Male Sex Drive: Definition, Factors, and Myths .
- If libido is the issue: When the “wanting” signal is muted, the most common upstream drivers are dopamine reward tone and testosterone permissive thresholds—see Dopamine and Libido and Testosterone and Libido in Men .
- If arousal/erection is the issue: When desire is present but erections fail, the problem often lives in blood-flow, nerves, or endothelial function—start with Erectile Dysfunction Hub .
What Is the Fundamental Distinction Between Libido and Arousal?
The fundamental distinction between libido and arousal is the difference between a proactive motivational state and a reactive physiological event.
To speak technically, scientists distinguish between “Incentive Salience” (the desire to act) and “Genital Tumescence” (the physical readiness to act) [LA8].
Incentive salience is the brain’s “go pursue this” signal; if you want the neurochemistry behind that motivational tagging, read Dopamine and Libido (incentive salience explained). Genital tumescence is the blood-flow response; when that fails, it behaves like a vascular/endothelial problem—see the Erectile Dysfunction Hub for the physical-mechanics side.
Defining Libido (The Mental Appetite)
Libido is the baseline “sexual drive” or appetite, operating as a psychological and emotional state of wanting or needing sexual intimacy [LA1].
It is driven largely by the brain’s reward system (Dopamine) and the baseline hormonal environment (Testosterone).
Levine distinguishes desire as a “biopsychosocial drive” that precedes the act itself. Essentially: Libido acts as the mental appetite for sex, initiating the pursuit of intimacy or fantasies.
Libido also presents in two common patterns—spontaneous (“out of the blue”) vs. responsive (“arousal-first”)—and knowing which one you run on changes what “low libido” actually means; compare: Spontaneous Libido in Men vs. Responsive Libido in Men.
Defining Arousal (The Physical Reaction)
Arousal is the immediate physical and psychological response to a specific sexual stimulus, whether tactile, visual, or mental [LA2]. It is driven by the autonomic nervous system triggering the release of Nitric Oxide to engorge the genitalia. Sexual arousal triggers the vascular filling of erectile tissue, resulting in a physical erection.
How Does the Biological “Engine” Differ for Libido and Arousal?
The biological “engine” differs in that Libido relies on slow-acting neuro-hormonal modulation, while Arousal relies on fast-acting vascular reflexes [LA3].
The Dual Control Model is the cleanest clinical way to explain why desire can be high one day and absent the next: it’s a balance between excitation and inhibition—see Dual Control Model (excitation vs inhibition) for the practical interpretation.
Think of Libido as the engine’s fuel mixture, which must be rich enough to run, and Arousal as the transmission and wheels that actually move the vehicle.
The Neuro-Hormonal Drivers of Libido
The primary drivers of Libido are Testosterone, which acts as a permissive fuel, and Dopamine, which acts as the motivational spark [LA5].
Libido is a “slow” system; it builds over time and is heavily influenced by lifestyle, sleep, and overall mood.
According to Pfaus [LA7], adequate testosterone levels support reward responsiveness, strengthening the subjective experience of sexual motivation.
Because testosterone and reward tone are sleep-sensitive, a “libido problem” is often a rhythm problem first; if morning desire disappeared after poor sleep, start with Sleep Deprivation and Libido (flattened testosterone rhythm).
The Vascular and Neural Drivers of Arousal
The primary drivers of Arousal are Nitric Oxide (NO) and the Parasympathetic Nervous System, which coordinate rapid vasodilation [LA2].
Unlike libido, Arousal is a “fast” system; it can happen in seconds in response to a trigger, even if baseline libido is low (reflexive arousal).
The AUA Guidelines confirm that this mechanism can function independently, leading to phenomena like “Morning Wood” or reflex erections [LA4].
Nitric oxide is the immediate chemical switch that relaxes smooth muscle and allows penile blood inflow; if erections are unreliable despite intact desire, review Nitric Oxide and Erections (vascular mechanism) to understand why “wanting” alone can’t overcome a blood-flow bottleneck.
Can You Experience Arousal Without Libido (and Vice Versa)?
You can experience arousal without libido, and vice versa, because desire pathways and genital reflex arcs can operate semi-independently.
This mismatch, known as Sexual Discordance, is a key diagnostic clue [LA8].
Scenario A: Libido Without Arousal (The “Will” but not the “Way”)
In this scenario, desire is present but erection quality is impaired—commonly classified under Erectile Dysfunction (ED) [LA4].
This is typically driven by vascular/endothelial issues, neurologic factors, or performance inhibition. The AUA confirms this state as a failure of the end-organ (penis) despite intact central signaling.
Effectively: High libido initiates arousal signaling, but is blocked by erectile-function impairment.
If desire is present but erection quality fails, that’s typically a hardware-side problem—use our Erectile Dysfunction Hub to triage vascular risk, medication effects, and nerve issues in a structured way.
Scenario B: Arousal Without Libido (The “Reaction” but not the “Urge”)
In this scenario, erections can occur via reflexive arousal, but Incentive Salience and motivation feel muted [LA8].
This often indicates hormonal imbalance (Low T), depression, or reward habituation (Dopamine Desensitization) [LA7].
Physical stimulation triggers a reflexive arousal response, but fails to engage the brain’s desire centers.
If erections can still occur but the urge is missing, that points upstream to motivation biology—start with Dopamine and Libido (reward tagging) and Testosterone and Libido (permissive threshold), because this pattern is usually “signal” more than “plumbing.”
What Common Factors Impact Libido vs. Arousal Differently?
Common factors impact libido and arousal differently depending on whether they target the brain’s reward center (Desire) or the body’s vascular system (Response).
Factors Impacting the “Desire” (Libido)
Factors impacting desire primarily affect neurochemistry and hormones, with Chronic Stress (Cortisol) often reducing sexual motivation [LA6].
Cortisol can suppress testosterone and dopamine, killing the mental drive. Low Testosterone primarily targets this “wanting” phase [LA5].
Cortisol is the classic libido suppressor because it raises inhibitory tone and can blunt reward sensitivity; if stress or burnout is the dominant context, see Cortisol and Libido (how stress becomes a brake).
Factors Impacting the “Response” (Arousal)
Factors impacting arousal most often involve vascular health and autonomic balance required for erectile function [LA4].
Acute alcohol consumption (“whiskey dick”) impairs the vascular response even if desire persists [LA2]. Acute anxiety triggers sympathetic inhibition (fight-or-flight), instantly shutting down the arousal mechanism.
Morning Erections (NPT) as a Practical Differentiator
Regular nocturnal or morning erections suggest core erection mechanics often remain intact, shifting suspicion toward psychogenic inhibition or libido context [LA4].
If the hardware works while you sleep (uninhibited state), but fails during intimacy, the issue is likely psychological (Libido/Anxiety) rather than structural (Arousal/Vascular).
Morning erections are a useful “hardware test” because they occur during sleep when performance anxiety is off; for interpretation (and when absence matters), see Morning Wood (NPT): What It Means Clinically.
[Checklist] Auditing Your Sexual Health: Libido vs. Arousal
Use this functional audit to determine if your primary issue lies with mental “wanting” (Libido) or physical “responding” (Arousal).
Functional and Health Audit
- ✓ Mental Check: Do you experience spontaneous sexual thoughts/fantasies? (If NO → Libido issue)
- ✓ Stimulus Check: Does direct stimulation trigger erection? (If NO → Arousal/Vascular issue)
- ✓ Morning Erection Check: Frequent morning erections? (If YES → Mechanics intact; investigate inhibition/desire)
- ✓ Stress Check: Chronic stress/exhaustion present? (Primarily kills Libido)
- ✓ Medication Audit: Taking SSRIs? (Can kill both Libido and Arousal).
- ! Safety Rule: Identifying the “Mind vs. Body” root cause is the first step to correct treatment.
If an SSRI is on board, libido and arousal can both drop through different mechanisms (motivation blunting + sexual side effects); use SSRI Sexual Side Effects (what’s reversible and what’s not) before assuming you “just have low testosterone.”
Choose the next page based on your pattern
- If you have desire but erections fail: follow the physical pathway in the Erectile Dysfunction Hub to assess vascular, nerve, and medication contributors.
- If erections happen but desire feels “offline”: start upstream with Dopamine and Libido and the threshold model in Testosterone and Libido in Men .
- If you’re unsure which you have: anchor the full framework first with Male Sex Drive: Definition, Factors, and Myths and then re-run the checklist on this page.
When to Seek Medical Help
Seek medical help if you experience persistent discordance or symptoms such as sudden libido loss, painful erections, or signs of cardiovascular disease.
Clinical References
- [LA1] Levine SB. (2002) “Reexploring the concept of sexual desire.” PubMed.
- [LA2] Dean RC, Lue TF. (2005) “Physiology of Penile Erection…” PMC.
- [LA3] Bancroft J, Janssen E. (2000) “The Dual Control Model of Male Sexual Response” PubMed.
- [LA4] Burnett AL, et al. (2018) “Erectile Dysfunction: AUA Guideline.” J Urol.
- [LA5] Bhasin S, et al. (2018) “Testosterone Therapy… Endocrine Society Guideline” JCEM.
- [LA6] Hamilton LD, et al. “Cortisol, sexual arousal, and affect…” PubMed.
- [LA7] Pfaus JG. (2009) “Pathways of sexual desire.” J Sex Med.
- [LA8] Toates F. “An integrative view of emotion and motivation…” PubMed.




One Response