Tight Foreskin (Phimosis): Symptoms, Complications, and Treatment Options
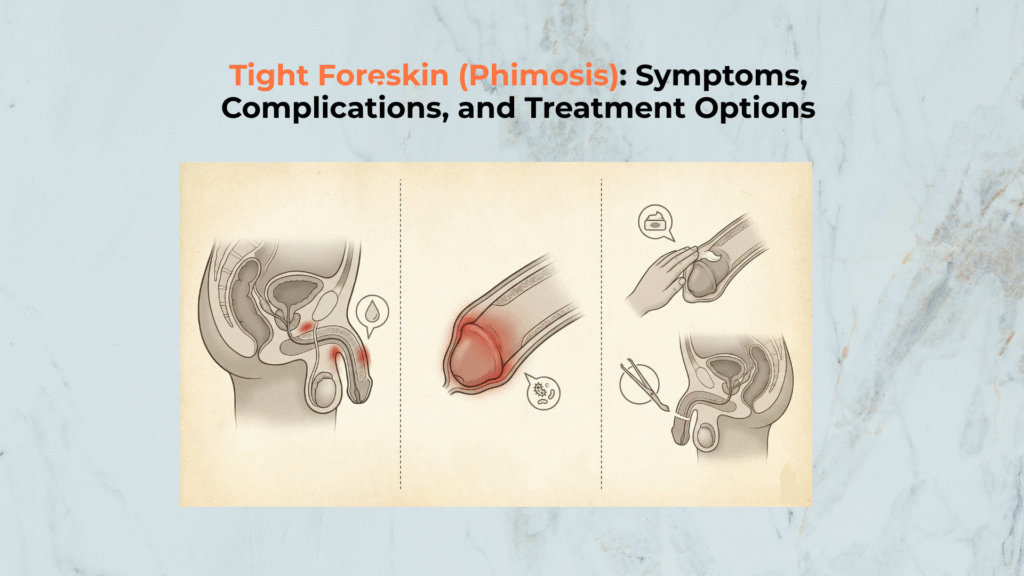
Phimosis is a clinical condition involving a tight foreskin that cannot be easily retracted, necessitating proper management to prevent mechanical complications such as painful erections and the emergency risk of Paraphimosis. The clinical anatomy behind retractability starts at the foreskin (prepuce), and the friction zone that becomes harder to clean is the corona + frenulum region. In your “types” layer, this pattern is tracked as a functional profile under tight foreskin (phimosis-type). This guide explains phimosis management in adolescents and adults, and clarifies normal non-retractability in children to prevent unnecessary manipulation [6, 8].
Important Medical Disclaimer
This guide is for educational purposes only. Phimosis should be managed by a urologist. If the retracted foreskin becomes swollen and cannot be returned to its normal position, the mechanism matches the same “trapped-behind-glans” dynamic explained in circumcision difference (retraction mechanics), and it requires emergency care immediately [3, 5].
Phimosis Management: At a Glance
- • Is it always pathological? No, it is often physiological in children.
- • Primary Risk: Mechanical pain and balanitis (glans inflammation) rise when cleaning becomes restricted.
- • Emergency: Paraphimosis becomes more likely when the tight ring is forced behind the glans in a way described in partially circumcised outcomes where residual skin can behave unpredictably during retraction.
- • Child Safety: Do not force retraction.
What Is Phimosis and How Is It Classified?
Defining Phimosis (The Constricting Ring)
Phimosis is defined as the inability of the prepuce to be fully retracted over the glans penis, and it is clinically classified into physiological and pathological types. The mechanical constriction occurs at the preputial orifice, the rim of tissue that forms the opening of the foreskin (prepuce). Clinical guidelines describe non-retractability as often physiological in childhood, with natural retractability increasing significantly as the child matures [6, 8]. This establishes the baseline for identifying when tightness becomes a clinical concern.
The Two Types: Physiological vs. Pathological
Phimosis is classified as either physiological (normal developmental) or pathological (acquired/scarred). Physiological Phimosis involves natural adhesions between the inner foreskin and the glans, which is standard in infants. Pathological Phimosis results from scarring or chronic inflammation where episodes of balanitis repeatedly reduce elasticity, and daily cleaning difficulty mirrors the care constraints described under an uncircumcised penis when retractability is limited [10, 13]. This acquired form rarely resolves without medical intervention.
Symptoms and Complications
Symptom 1: Painful Erections and Intercourse
The most significant symptom for adults is painful erections (dyspareunia) caused by mechanical stress on the tight tissue. The glans expands during arousal, forcing the inelastic preputial orifice to stretch beyond its threshold, which can lead to micro-tearing. When tightness blocks cleaning at the coronal sulcus region, the pattern commonly escalates into recurrent balanitis [9, 10]. Persistent mechanical stress results in increased scarring, which further narrows the opening over time.
Complication 1: Paraphimosis (Medical Emergency)
Paraphimosis is a true urologic emergency occurring when the tight foreskin is retracted but cannot be returned to its neutral position. The constricted ring impairs venous and lymphatic outflow, causing massive swelling of the glans penis [3, 4]. Immediate professional evaluation is required to manually restore circulation.
What Are the Treatment Options?
Treatment 1: Topical Steroid Creams
Topical Steroid Creams are the standard first-line conservative approach to increase foreskin elasticity. High-potency corticosteroids are applied directly to the tight ring to reduce inflammation and aid in tissue remodeling. Where steroids fail and the opening remains functionally obstructive, the tissue-removal endpoint aligns with the exposure state described in a circumcised penis, while tissue-preserving outcomes can resemble the mixed-coverage pattern in a partially circumcised penis. A 2024 Cochrane review found that topical corticosteroids significantly increased complete resolution after 4–8 weeks compared to placebo [1]. This method tends to be successful in many cases, especially when combined with gentle stretching exercises.
Treatment 2: Surgical Correction (Definitive Solution)
Surgical correction is considered the definitive solution for severe or recurrent Phimosis that fails conservative therapy. Circumcision permanently removes the constricted tissue, producing the exposed-glans baseline described in a circumcised penis, while tissue-preserving options are still organized around the original foreskin anatomy. Urological guidelines recommend surgical intervention when Phimosis is refractory to steroids or when Lichen Sclerosus is suspected [10, 13]. Surgical options guarantee the elimination of mechanical constriction at the preputial orifice.
When to Consult a Doctor (Safety Triage)
Seek medical evaluation whenever Phimosis causes pain, bleeding, or recurrent infection, or if the skin becomes trapped. Recurrent redness or discharge that matches balanitis is a common signal that cleaning limitations have progressed beyond the normal hygiene constraints described for an uncircumcised penis when retractability is reduced, which is why this profile is captured under tight foreskin (phimosis-type).
Clinical Red Flags
- ⚠ Retraction Pain: Pain or “restriction” during erection or activity [6, 10].
- ⚠ Recurring Infection: Redness or discharge beneath the skin that aligns with balanitis [9].
- ⚠ Scarring: White, waxy, or warty-looking skin changes (Lichen Sclerosus) [13].
- 🚨 EMERGENCY: If the glans is swollen and the foreskin cannot be returned to its normal position, the trapped-ring mechanism is clinically consistent with paraphimosis and requires emergency care immediately [3, 5].
Frequently Asked Questions
Can phimosis be cured without surgery?
Yes. A combination of high-potency topical steroid creams and gentle stretching exercises resolves the condition in a significant number of patients, avoiding the need for circumcision.
Does tight foreskin affect hygiene?
Yes. Inability to retract the foreskin makes cleaning the glans difficult, allowing debris to accumulate around the corona / sulcus zone, which increases the risk of balanitis.
Can I have sexual intercourse with phimosis?
It is possible but often painful; erection stretches the tight ring and can cause micro-tears, and the “stuck-behind-glans” risk is anatomically defined by the glans and retracting foreskin interface.
Is circumcision the only surgical option?
No. Preputioplasty (surgical widening) is a tissue-preserving alternative that relieves the tightness while keeping the foreskin intact. However, circumcision is often preferred if scarring (BXO) is severe.
Conclusion: Sustaining Integrated Care
In conclusion, Phimosis is a highly treatable condition that requires a distinction between normal development and pathological tightening to ensure effective management. Management ranges from conservative steroid applications to definitive surgical correction that can shift anatomy toward the circumcised state, while mild cases still follow the cleaning constraints described for an uncircumcised state within the penis-types hub. Crucially, do not force retraction in children and seek care for adult pain or paraphimosis.
Final Checklist
FBU Clinical AI
Powered by OpenAIHi there! 👋 I’m analyzing the guide in real-time. Ask me specific questions about Phimosis, or feel free to chat naturally!