Cold-Glans Penis: Circulation, Temperature, and Sexual Health
Analyzing Hemodynamics, Sensitivity, and Vascular Normality
Cold-Glans Penis is a physiological thermal state—not a disease entity. It is a normal characteristic dictated by differential hemodynamics between the glans and the shaft.
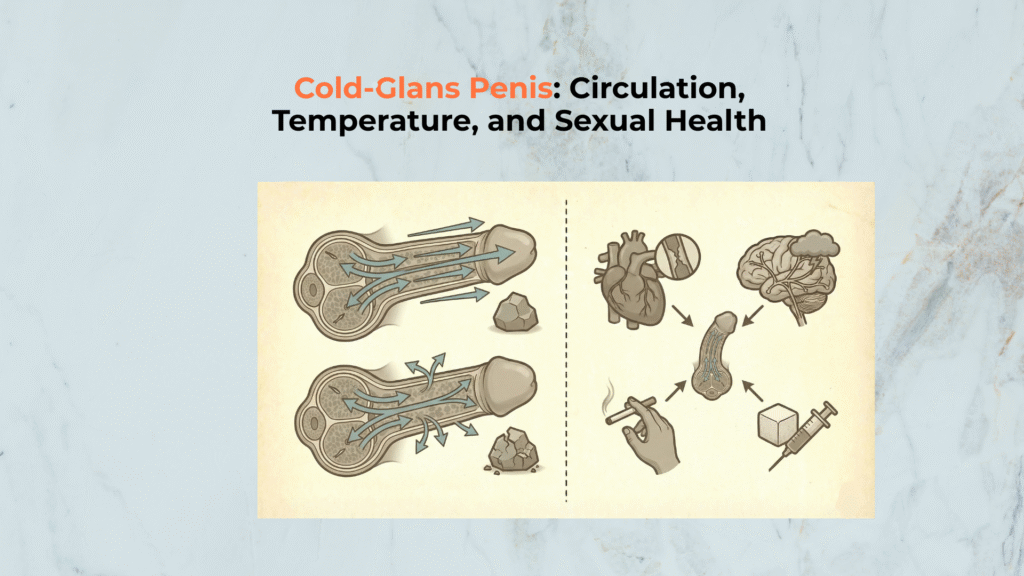
This indicates a difference in blood flow and heat retention, not poor health or low sensitivity. The phenomenon is fundamentally due to anatomical differences between the Corpus Spongiosum (which forms the glans) and the Corpora Cavernosa (which forms the shaft) [C1].
Important Medical Disclaimer
A Cold-Glans Penis is typically normal.
WARNING: If the coldness is accompanied by pain, discoloration (blue/white/black), or systemic coldness in the fingers/toes, consult a physician immediately to rule out underlying vascular issues like Raynaud’s Phenomenon or ischemia [C8, C10].
What Is the Anatomical Cause of a Cold-Glans Penis?
The anatomical cause of a Cold-Glans Penis is the difference in vascular structure and pressure between the glans and the adjacent shaft.
Defining the Phenomenon (Temperature Gradient)
The phenomenon is defined as a temperature difference where the Glans Penis feels noticeably colder to the touch than the adjacent Shaft (Corpora Cavernosa), especially in the flaccid state.
While injury often presents with heat and redness, this cooling effect is passive. Crisostomo-Wynne et al. demonstrated via thermographic measurement that the penis averages:
- ~34.7°C in the flaccid state.
- ~36.1°C in the erect state [C4].
This supports that a “cold then warm” pattern is normal and establishes the gradient as a localized, physiological event rather than a systemic failure.
The Premise: The Low-Pressure Spongiosum
The low-pressure operation of the Corpus Spongiosum forms the anatomical premise for the Cold-Glans Penis. Unlike the cavernosa, the glans acts as a low-pressure vascular cushion designed to protect the urethra during ejaculation.
Dean & Lue explain that the low-pressure sinusoids of the glans and its thin tunica result in minimal venous occlusion compared to the rigid shaft [C1]. This anatomical difference explains why heat retention is significantly lower in the flaccid state.
A cold glans is usually a pressure + flow difference between erectile compartments, so start with spongiosum vs cavernosa to see why the glans (spongiosum) behaves like a low-pressure cushion while the shaft (cavernosa) retains heat.
How Does Blood Flow Differentially Affect Glans Temperature?
Blood flow differentially affects glans temperature by creating passive cooling in the flaccid state and aggressive thermal input during the erection cycle.
Flaccid State Hemodynamics
In the flaccid state, Hemodynamics cause the glans to act like a slight cooling system due to continuous, low-volume drainage. Blood drains continuously through the spongy tissue, allowing heat to escape through the exposed skin surface.
The lack of a thick, insulating tunica albuginea means heat is not trapped efficiently in the spongiosum [C1].
The Temperature Change During Erection
The temperature of the glans rapidly normalizes and reverses during the erection cycle. Arousal floods the glans via the Bulbourethral and Dorsal Arteries [C2].
According to Torenvlied et al., the massive increase in blood inflow rapidly raises tissue temperature, making the glans feel warm to the touch [C5]. This dynamic shift—from cool to warm—is the primary sign of healthy vascular function.
The “cold then warm” pattern depends on state switching, and the clearest mechanism map is flaccid vs erect blood flow because glans temperature normalizes when arterial inflow surges during erection.
Anatomical Detail: The Independent Supply
To understand why the glans can be cold while the shaft is warm (or vice versa), one must visualize the arterial plumbing. The glans is primarily fed by the Dorsal Artery and the Urethral Artery, whereas the shaft’s heat comes mainly from the Deep Arteries. This separation allows for distinct thermal states.
If you’re trying to understand why the glans can feel cooler even when the shaft feels warm, anchor the plumbing through the vascular pathway which separates glans supply from cavernosa filling and explains “different temperatures, same organ.”
Is a Cold-Glans Penis a Sign of Poor Health or Low Sensitivity?
A Cold-Glans Penis is not a sign of poor health or low sensitivity unless specific pathological symptoms are present.
Link to Sexual Health (Not Pathological)
A cold glans is a normal physiological state that does not indicate poor sexual health in the absence of other symptoms. The key functional test is warming:
- If the glans warms with erection, the vascular supply is functional.
- Temperature alone is rarely a diagnostic marker for ED.
NIAMS and SMSNA confirm that clinical concern is reserved for cases where the glans fails to warm and presents with pain, pallor, or blackening [C8, C10].
If the glans does not warm with erection and the pattern overlaps with firmness loss, route the reader to venous leak type because persistent outflow can prevent full engorgement even when arousal is present.
Link to Sensitivity (Minimal Impact)
The temperature difference has minimal or no lasting impact on the glans’s high sensitivity.
Sensation is governed by the Dorsal Nerve of the Penis, which is distinct from the vascular supply.
According to Weech (NCBI), the dorsal nerve acts as the terminal branch of the pudendal nerve, ensuring sensation remains intact regardless of surface temperature [C7].
Any transient numbness from cold dissipates immediately upon arousal.
Sensation is not controlled by surface temperature, so connect the sensitivity claim to the dorsal nerve to understand why a cool glans can still feel highly sensitive when the sensory pathway is intact.
When Should You Worry About a Cold-Glans Penis?
You should worry about a Cold-Glans Penis only if the coldness is a symptom of a systemic vascular issue or accompanied by pain and numbness.
1. Systemic Vascular Issues
Systemic Vascular Issues are the primary pathological concern when coldness occurs in a specific pattern known as Raynaud’s Phenomenon.
This presents as coldness accompanied by discoloration (white/blue/red sequence) and often affects fingers or toes. Kropman [C9] confirms penile Raynaud’s exists. Immediate medical assessment is required if this pattern appears.
2. Pain and Numbness
The simultaneous presence of pain and profound numbness is a key clinical red flag indicating potential ischemia.
Worry if the coldness is accompanied by darkening of the tissue (blue/black) or intense pain. SMSNA [C10] states these symptoms suggest Penile Glans Necrosis, a medical emergency. Normal coldness is never painful.
[Checklist] Functional Audit for the Cold-Glans Penis
Use this functional audit checklist to determine if your Cold-Glans Penis exhibits normal vascular characteristics.
- ✓
- ?
- !
-
XSafety Rule Do NOT use external heat sources (heating pads) to warm the glans; this causes burn injury [C11].
Conclusion
In conclusion, the Cold-Glans Penis is a harmless, normal thermal characteristic dictated by the low-pressure hemodynamics of the Corpus Spongiosum, which is functionally distinct from the Shaft.
“Physiological literacy prevents unnecessary health anxiety. Your temperature gradient is a sign of normal vascular efficiency.”
Scientific References
- [C1] Dean RC, Lue TF. (2005) “Physiology of Penile Erection…” PMC
- [C2] BUMC Sexual Medicine. “Male Genital Anatomy” BUMC
- [C3] Panchatsharam PK. “Physiology, Erection” StatPearls
- [C4] Crisostomo-Wynne T, et al. (2021) “Use of Thermographic Imaging…” AUA/Lippincott
- [C5] Torenvlied HJ, et al. (2024) “‘Staying Hot’: influence of overnight…” BJUI
- [C6] Fogarty JD, et al. (2005) “Cutaneous temperature measurements…” PubMed
- [C7] Weech D. (2023) “Anatomy, Abdomen and Pelvis, Penis Dorsal Nerve” NCBI Bookshelf
- [C8] NIAMS (NIH). “Raynaud’s Phenomenon: Symptoms…” NIAMS
- [C9] Kropman RF. (2004) “Raynaud’s phenomenon of the penis” PubMed
- [C10] SMSNA. “Penile Glans Necrosis – A Look into the Rare Condition” SMSNA
- [C11] Jabir S, et al. (2013) “Burn Injuries Resulting from Hot Water Bottle Use” PMC