What Is Balanitis? A Complete Guide to Causes, Symptoms, and Treatment
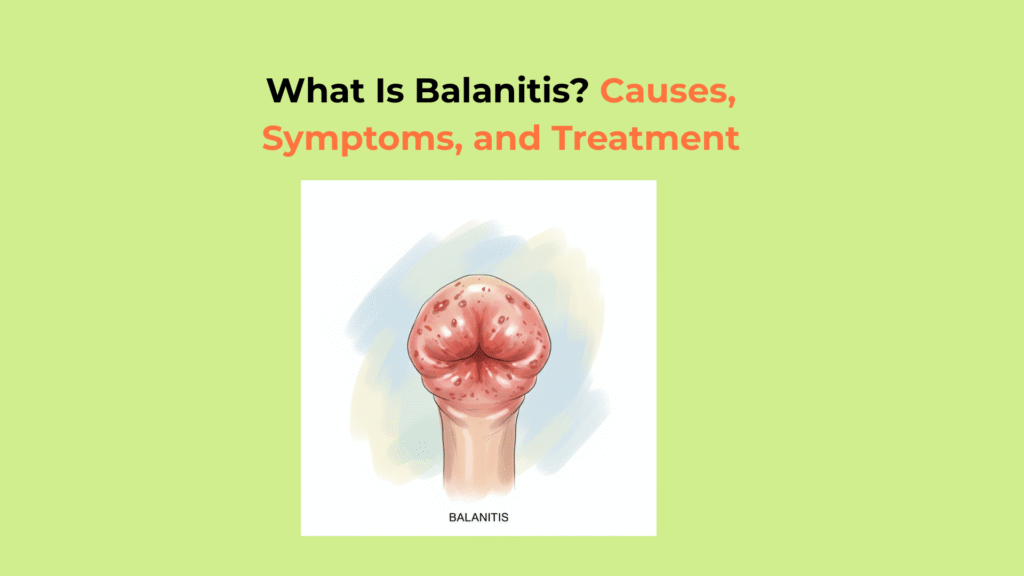
Balanitis is the medical term for inflammation, soreness, or swelling of the glans (head of the penis), a common condition most often caused by poor hygiene in uncircumcised men or by a yeast infection.
While the symptoms of balanitis can be alarming, it is a common and treatable condition, making a clear, factual guide essential. This guide provides a clear, step-by-step framework to understand what balanitis is, its common causes, how to identify its symptoms, and the most effective treatment options.
Understanding the specific nature of balanitis is the first step toward managing it effectively.
What Is Balanitis? (Defining the Central Entity)
Balanitis is clinically defined as an inflammation of the glans penis (the head of the penis), a common condition that is not an STI itself but can sometimes be caused by one.
Understanding Balanitis vs. Balanoposthitis
Balanitis must be distinguished from Balanoposthitis; Balanitis involves inflammation of the glans only, while Balanoposthitis involves inflammation of both the glans and the foreskin (prepuce).
This distinction is important for a clinician when determining the extent of the condition and the most appropriate treatment. While balanitis affects only the head of the penis, balanoposthitis indicates the inflammation has also spread to the overlying foreskin.
Who Is Most at Risk for Developing Balanitis?
The individuals most at risk for developing balanitis are uncircumcised men with poor hygiene, as the foreskin can trap moisture and pathogens, and men with underlying health conditions, especially uncontrolled diabetes.
Balanitis is estimated to affect up to 1 in 10 uncircumcised men at some point in their life (Source: StatPearls, NCBI). The primary risk factors include:
- Uncircumcised Status: The foreskin can trap moisture, heat, and skin cells, creating an ideal environment for yeast and bacteria to thrive.
- Poor Hygiene: This leads to the buildup of smegma, which can irritate the skin and harbor microorganisms.
- Diabetes Mellitus: Uncontrolled diabetes can lead to high blood sugar, which results in glucose (sugar) in the urine. This glucose feeds yeast, promoting overgrowth.
- Phimosis: This is a condition defined as a tight foreskin that cannot be retracted, which makes proper cleaning of the glans impossible.
What Are the Common Symptoms of Balanitis?
The common “symptoms of balanitis” include primary physical signs like redness, swelling, and itching on the glans, and may be associated with discharge, odor, or pain.
The Primary Physical Symptoms of Balanitis
The primary physical “symptoms of balanitis” are localized inflammation and irritation on the head of the penis.
- Redness and swelling on the head of the penis (glans)
- Pain, soreness, or tenderness
- Itching or irritation
Other Associated Symptoms of Balanitis
Other associated “symptoms of balanitis” often include a thick, lumpy discharge (smegma) under the foreskin, an unpleasant odor, pain during urination, or phimosis.
- A thick, lumpy discharge (smegma) under the foreskin
- An unpleasant odor
- Pain or difficulty when urinating
- Phimosis (inability to retract the foreskin), which can be a new symptom caused by the swelling
When to See a Doctor for Balanitis Symptoms
You should see a doctor for “balanitis symptoms” if they are severe, do not improve with basic hygiene after 2-3 days, are recurrent, or are accompanied by fever, severe pain, or an inability to urinate.
A professional diagnosis is essential to rule out more serious conditions, such as certain STIs, and to identify an underlying cause like diabetes mellitus.
What Are the Main Causes of Balanitis? (Exploring the Root Factors)
The main “causes of balanitis” are diverse and are categorized as infectious (most commonly a yeast infection), non-infectious irritants (like harsh soaps), poor hygiene (especially under a foreskin), and underlying health conditions like diabetes.
Infectious Causes of Balanitis (The Most Common)
Infectious agents are the most common “causes of balanitis,” with the yeast Candida albicans being the most frequent culprit, followed by bacterial infections and some STIs.
- Yeast Infection (Candida): This is the most common cause of balanitis. Candida albicans is a fungus that naturally lives on the skin, but it can overgrow in warm, moist conditions, often presenting with a red, itchy rash and clumpy white discharge.
- Bacterial Infection: Bacteria like Staphylococcus or Streptococcus can also cause balanitis, especially if hygiene is poor or the skin is broken.
- Sexually Transmitted Infections (STIs): While balanitis itself isn’t an STI, infections like herpes, gonorrhea, or syphilis can present with symptoms of inflammation on the glans.
Non-Infectious Irritant Causes of Balanitis
Non-Infectious “causes of balanitis” include chemical irritation from common household or personal products that disrupt the sensitive skin of the glans. Common irritants include harsh soaps, shower gels, unscented lubricants, latex condoms, or residual laundry detergents on underwear.
Poor Hygiene as a Cause of Balanitis
Poor hygiene, particularly in uncircumcised men, is a primary cause of balanitis due to the buildup of smegma under the foreskin.
Smegma is a natural lubricant made of dead skin cells and oil. If not cleaned away regularly, this buildup creates an ideal, warm, moist environment for bacteria and fungi to grow, which directly leads to inflammation.
Underlying Health Conditions That Cause Balanitis
Underlying health conditions are a key cause of recurrent balanitis, most notably uncontrolled diabetes and anatomical issues like phimosis.
High blood sugar levels in people with uncontrolled diabetes can lead to glucose (sugar) in the urine. When urine passes over the glans, this glucose provides a rich food source for yeast (Candida) to overgrow, causing recurrent infections.
Phimosis, defined as a tight foreskin that cannot be retracted, makes proper cleaning impossible. This inevitably leads to the buildup of smegma and pathogens, causing chronic or recurrent balanitis.
How Is Balanitis Diagnosed by a Healthcare Provider?
Balanitis is diagnosed by a healthcare provider through a physical examination and a review of your symptoms and history, often followed by simple diagnostic tests to pinpoint the exact cause.
The Diagnostic Process for Balanitis: What to Expect
The diagnostic process for balanitis starts with a visual examination of the glans and foreskin, followed by a confidential discussion of your symptoms, hygiene practices, and sexual history. Your doctor will look for redness, swelling, and discharge and check for phimosis.
Diagnostic Tests to Determine the Cause of Balanitis
The most common diagnostic tests to determine the specific “cause of balanitis” include a swab test for infections, a urine test for diabetes, or a blood test.
- Swab Test: A doctor may take a sample of any discharge from under the foreskin. This sample is sent to a lab to test for bacteria, fungi (Candida), or STIs.
- Urine Test: This test is used to check for signs of infection or, more importantly, for glucose in the urine, which strongly suggests diabetes.
- Blood Test: A blood test may be ordered to check blood sugar levels if diabetes is suspected as the underlying cause of recurrent balanitis.
What Are the Most Effective Treatments for Balanitis?
The most effective “treatments for balanitis” depend on the specific cause and range from simple hygiene improvements and at-home care to prescription topical creams that target the underlying infection or inflammation.
At-Home & Hygiene Treatments for Balanitis
Effective at-home “treatment for balanitis” involves stopping the use of all potential irritants and practicing good hygiene by gently washing the penis with warm water only and patting it dry.
- Gently wash the penis with warm water only (no soap) and pat dry.
- Avoid all potential irritants, including soaps, lotions, and fragranced products.
- Practice good hygiene: If uncircumcised, gently retract the foreskin to clean the glans daily, then dry the area before replacing the foreskin.
Medical Treatments: Topical Creams for Balanitis
Medical “treatment for balanitis” is targeted to the diagnosed cause and typically involves an antifungal cream for yeast, an antibiotic for bacteria, or a mild steroid cream for irritation.
- Antifungal Cream (e.g., clotrimazole): This is the standard balanitis cream for infections caused by a Candida yeast infection.
- Antibiotic Cream or Pills (e.g., mupirocin): These are prescribed for balanitis caused by a bacterial infection.
- Mild Steroid Cream (e.g., hydrocortisone): This may be recommended to reduce inflammation and itching caused by non-infectious irritants or allergies.
Treating the Underlying Cause of Recurrent Balanitis
Treating recurrent balanitis requires managing the underlying cause, such as improving blood sugar control for diabetes or addressing anatomical issues like phimosis. If balanitis keeps returning, your doctor will focus on treating these root-cause issues.
Circumcision as a Treatment for Chronic Balanitis
Circumcision, the surgical removal of the foreskin, may be recommended as a permanent “treatment for balanitis” in men who suffer from severe, chronic, or recurrent infections, or in cases caused by phimosis. Medical bodies like the American Urological Association (AUA) recognize circumcision as a highly effective option for preventing recurrent balanitis as it removes the environment where pathogens grow (Source: AUA Guideline).
Comparing Common Balanitis Topical Treatments
This table compares the most common topical “treatments for balanitis,” their target cause, and their mechanism of action.
| Treatment Type | Target Cause | Example | Action |
|---|---|---|---|
| Antifungal Cream | Yeast (Candida) | Clotrimazole | Kills the fungal infection. |
| Antibiotic Cream | Bacteria | Mupirocin | Kills the bacterial infection. |
| Steroid Cream | Irritation / Allergy | Hydrocortisone 1% | Reduces inflammation and itching. |
Key Takeaways: Your Action Plan for Managing Balanitis
Your action plan for managing balanitis involves identifying symptoms, starting basic at-home care, seeking a professional diagnosis to find the cause, using the correct medical treatment, and addressing any underlying health issues.
Glossary of Clinical Terms
To ensure full clarity, this glossary defines the key clinical and scientific terms used throughout this guide on balanitis.
| Term | Definition |
|---|---|
| Balanitis | Inflammation, redness, and swelling of the glans (head of the penis). |
| Balanoposthitis | Inflammation that involves both the glans (head of the penis) and the foreskin. |
| Glans | The sensitive, cone-shaped head or tip of the penis. |
| Smegma | A natural, cheese-like substance made of dead skin cells and oils that can build up under the foreskin. |
| Candida albicans | A type of yeast (fungus) that is the most common infectious cause of balanitis. |
| Phimosis | A condition in uncircumcised males where the foreskin is too tight to be retracted back over the glans. |
Conclusion
In conclusion, balanitis is a common and highly treatable inflammation of the glans penis, most often caused by a simple yeast infection or poor hygiene, which can be quickly resolved with a proper medical diagnosis and the correct topical treatment. A medical diagnosis is key to getting the right cream (antifungal, antibiotic, or steroid) to treat the specific cause.
At factbasedurology, we believe that providing clear, factual information on common conditions like balanitis is the best way to reduce anxiety and encourage prompt, effective care. Understanding the causes of balanitis is the first step toward treating it quickly and preventing it from returning.




6 Responses