How Is Blood Drained from the Corpora Cavernosa?
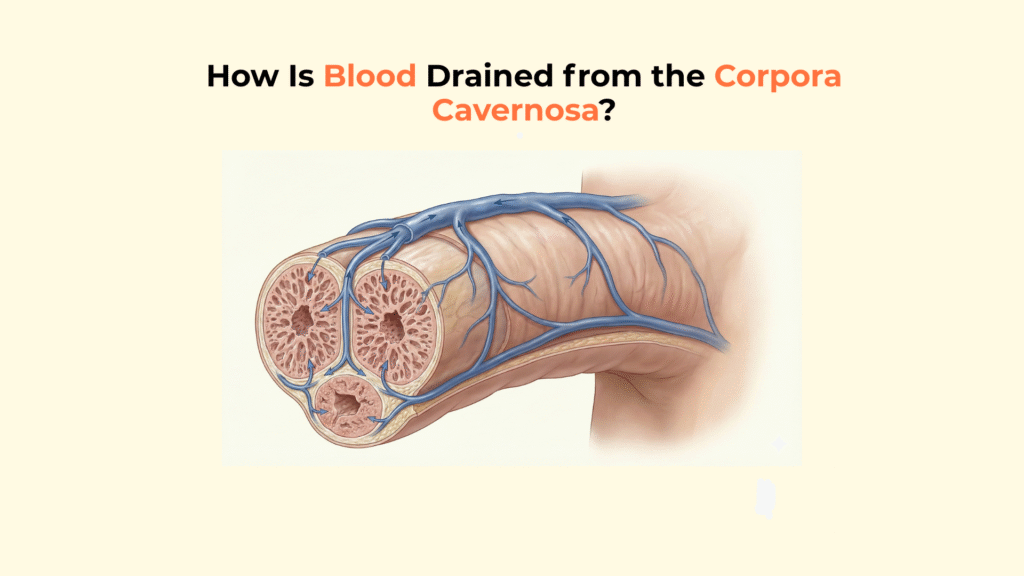
Blood is drained from the corpora cavernosa through a specialized system beginning at the sub-tunical venular plexus, exiting via emissary veins, and primarily converging into the deep dorsal vein of the penis.
Unlike standard circulatory pathways where flow is continuous, this drainage system is anatomically unique because it is designed to be obstructed during sexual arousal. The venous outflow must be significantly restricted to maintain high intracavernosal pressure, allowing for penile rigidity.
This guide provides a detailed anatomical map of the penile venous system, tracing the drainage from the microscopic venules to the major veins, and explaining the critical veno-occlusive mechanism.
Important Medical Disclaimer
This information is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Consult with a qualified healthcare provider regarding any medical condition or concerns about your health.
Key Vascular Facts: Penile Veins
The Origin: Drainage starts at the tiny sub-tunical venular plexus under the Tunica Albuginea.
The Exit: Blood leaves through emissary veins that pierce the tunica.
The Deep Dorsal Vein: The main highway for drainage from the glans and corpora cavernosa.
The Superficial Dorsal Vein: Drains the skin and dartos fascia, NOT the erectile tissue.
The Mechanism: During erection, the expanding tissue crushes the sub-tunical venules, trapping blood inside.
Where Does the Venous Drainage of the Corpora Cavernosa Begin?
The venous drainage of the corpora cavernosa begins at the microscopic level with the sub-tunical venular plexus, a network of tiny venules located immediately beneath the rigid Tunica Albuginea.
The Sub-Tunical Venular Plexus (The Collection Zone)
These venules function as the primary collection zone, gathering blood from the peripheral sinusoids of the erectile tissue. Structurally, they are positioned in a vulnerable location. Because they are sandwiched between the expanding erectile tissue (sinusoids) and the non-compliant, rigid tunica albuginea, they are easily compressed.
This anatomical positioning is not a design flaw but a functional necessity; it is the fundamental mechanical key to maintaining an erection.
Interactive 3D Simulation
The Compression Chamber: Observe the blue venules flatten as red tissue expands.
The Emissary Veins (The Exit Bridges)
The emissary veins arise from the sub-tunical plexus and pierce obliquely through the layers of the Tunica Albuginea to exit the erectile bodies. In clinical anatomy, these veins act as the “doors” or bridges out of the high-pressure chamber.
Upon exiting the tunica, they merge to form the Circumflex Veins, which encircle the shaft laterally before feeding into the larger Deep Dorsal Vein.
What Are the Major Pathways for Venous Drainage from the Penis?
The major pathways for venous drainage include the Deep Dorsal Vein (the primary drain for erectile tissue), the Cavernosal Veins, and the Superficial Dorsal Vein (which drains the skin).
The Deep Dorsal Vein (The Primary Highway)
The Deep Dorsal Vein is formed by the convergence of the Circumflex Veins and runs along the midline dorsal groove of the penis, deep to Buck’s Fascia. It serves as the main conduit for deoxygenated blood leaving the erectile chambers.
It is responsible for the majority of the drainage from the glans and the distal two-thirds of the corpora cavernosa. The Deep Dorsal Vein eventually empties into the Periprostatic Plexus (also known as Santorini’s Plexus). For a comprehensive review of this anatomy, refer to this NIH Review of Penile Anatomy.
The deep dorsal vein that collects blood from the emissary veins runs within the same fascial compartment as key sensory structures such as the dorsal penile nerve, explaining why surgical trauma in this region can affect both sensation and venous outflow.
The Cavernosal and Crural Veins (The Deep Roots)
The Cavernosal and Crural Veins drain the proximal (root) sections of the Corpora Cavernosa and the crura. Unlike the dorsal system, these veins exit at the base of the penis. They provide essential drainage for the anchored roots of the penis located behind the pubic bone. These vessels drain directly into the Internal Pudendal Vein.
At the root of the penis, additional venous drainage pathways emerge from the crura, which are anchored to the pelvis by the same structures described in the pelvic attachment system, allowing proximal venous blood to bypass the dorsal route entirely.
The Superficial Dorsal Vein (The Skin Drain)
The Superficial Dorsal Vein is distinct because it lies outside Buck’s Fascia and drains the skin and dartos fascia, not the erectile tissue. It is critical to distinguish this vessel from the deep system. This vein is responsible for the visible blue veins often seen on the surface of the penile skin. It drains superiorly into the External Pudendal Vein, connecting to the Saphenous system, and plays no role in the mechanics of erection.
How Is Venous Drainage Stopped During Erection (Veno-Occlusion)?
Venous drainage is stopped during erection by the veno-occlusive mechanism, a passive process where expanding erectile tissue mechanically compresses the veins against the Tunica Albuginea.
The drainage efficiency of the corpora cavernosa is inseparable from how blood first enters through the helicine arteries, since venous outflow can only be mechanically restricted if arterial inflow has already expanded the sinusoidal spaces.
These sinusoids are embedded within the paired erectile chambers known as the corpora cavernosa, whose expansion is what physically compresses the sub-tunical venules during erection.
The Passive Compression Mechanism
The drainage system does not have active muscular valves; instead, it relies entirely on passive mechanical compression generated by internal pressure.
The physiological sequence is specific: the expansion of the sinusoids (Entity) compresses the sub-tunical venules against the tunica albuginea (Action), mechanically blocking venous outflow (Result). This explains why the penis stays hard without constant pumping; the blood is effectively trapped by the pressure of the erection itself.
The passive compression described in the veno-occlusive mechanism depends heavily on the structural stiffness of the tunica albuginea, which acts as the non-yielding surface against which venous channels are flattened.
Although venous occlusion is a mechanical process, it cannot occur unless the surrounding trabecular smooth muscle has fully relaxed to allow sinusoidal expansion in the first place.
The Role of the Emissary Veins in Occlusion
As the emissary veins pass obliquely through the layers of the Tunica Albuginea, the stretching of the tunica effectively “kinks” or “pinches” them shut. If the smooth muscle of the corpora cavernosa fails to relax sufficiently, or if the tunica loses elasticity, the emissary veins may not be fully compressed.
This failure allows blood to escape, a condition known as Venous Leak, which is a primary cause of Erectile Dysfunction. For further reading on the hemodynamics of this failure, see this study on Venous Leak Mechanisms.
When venous drainage fails to shut down properly, blood escapes prematurely through the dorsal system and contributes to erectile dysfunction, even when arterial inflow is otherwise intact.
In fibrotic disorders such as Peyronie’s disease, deformation of the tunica alters the geometry of sub-tunical venules, disrupting normal venous compression and leading to asymmetric rigidity.
Comparative Matrix: Penile Venous Drainage Systems
This table provides a direct comparison of the three major venous pathways, detailing their drainage source, anatomical depth, and destination.
| Vein | Drainage Source | Anatomical Depth | Destination |
|---|---|---|---|
| Deep Dorsal Vein | Corpora Cavernosa, Glans | Deep to Buck’s Fascia | Periprostatic Plexus |
| Superficial Dorsal Vein | Skin, Dartos Fascia | Superficial to Buck’s Fascia | External Pudendal Vein |
| Cavernosal/Crural Veins | Proximal Crura | Deep Perineum | Internal Pudendal Vein |
[Checklist] Identifying the Venous Drainage
- Starting Point: Is the Sub-Tunical Plexus identified as the origin?
- The “Pinch”: Is the compression of veins against the Tunica Albuginea explained?
- Major Route: Is the Deep Dorsal Vein identified as the primary drain for the shaft?
- Distinction: Is the Superficial Dorsal Vein correctly identified as draining skin, not erectile tissue?
- Destination: Is the Periprostatic Plexus identified as the endpoint for the Deep Dorsal Vein?
Glossary of Anatomical Terms
- Deep Dorsal Vein
- The main vein that drains the erectile tissue, located deep within the penis under Buck’s fascia.
- Superficial Dorsal Vein
- The vein visible under the skin that drains the skin and superficial layers of the penis.
- Sub-Tunical Venular Plexus
- A network of tiny veins just under the tunica albuginea where drainage begins.
- Emissary Veins
- Veins that pass through the tunica albuginea to carry blood out of the erectile tissue.
- Periprostatic Plexus
- A network of veins around the prostate where the deep dorsal vein drains.
- Veno-Occlusive Mechanism
- The process of trapping blood in the penis by compressing veins to maintain an erection.
Frequently Asked Questions
1. What is the primary vein responsible for draining the erection?
The Deep Dorsal Vein, which runs along the top of the shaft deep to Buck’s fascia.
2. How does the penis trap blood to maintain an erection?
Expanding erectile tissue compresses the sub-tunical veins against the rigid Tunica Albuginea, mechanically blocking outflow.
3. What is the difference between the superficial and deep dorsal veins?
The superficial vein drains the skin and is visible externally; the deep vein drains the erectile tissue and is critical for function.
4. What are emissary veins?
Small veins that pierce obliquely through the Tunica Albuginea to transport blood from the erectile tissue to the deep dorsal vein.
5. Do penile veins have valves like leg veins?
Generally no; the drainage control relies entirely on the passive mechanical compression of the tunica.
6. What is a “venous leak”?
A form of erectile dysfunction where the veno-occlusive mechanism fails to trap blood effectively, often due to tunica or smooth muscle issues.
7. Where does the sub-tunical venular plexus sit?
It is sandwiched immediately between the soft erectile tissue (sinusoids) and the hard outer shell (Tunica Albuginea).
8. Where does the deep dorsal vein empty into?
It drains primarily into the Periprostatic Plexus (Santorini’s Plexus) located behind the pubic bone.
9. Does the superficial dorsal vein affect erectile rigidity?
No, it drains the skin and dartos fascia and plays no mechanical role in maintaining erection rigidity.
10. Why is venous drainage obstructed during sexual arousal?
To convert the penis from a circulatory organ into a high-pressure hydraulic unit capable of penetration.
Conclusion
In conclusion, the drainage of blood from the corpora cavernosa is a highly regulated process involving a specialized network of deep veins and a mechanical “pinch” system that is essential for maintaining erection rigidity.
By understanding the progression from the Sub-Tunical Plexus through the Emissary Veins to the Deep Dorsal Vein, we gain insight into how the body manages blood volume during sexual function. The veno-occlusive mechanism ensures that this drainage is temporarily halted, turning a circulatory system into a hydraulic one.
Once blood exits the deep dorsal vein, it joins the larger pelvic venous network described within the broader penile vascular pathway, completing the transition from intracavernosal pressure to systemic venous return.
At Factbasedurology, we believe that understanding your body’s plumbing is the first step to mastering your health. This elegant balance of inflow and restricted outflow is the physiological secret to sexual function.