What Is Peyronie’s Disease? Causes, Symptoms, and Treatment
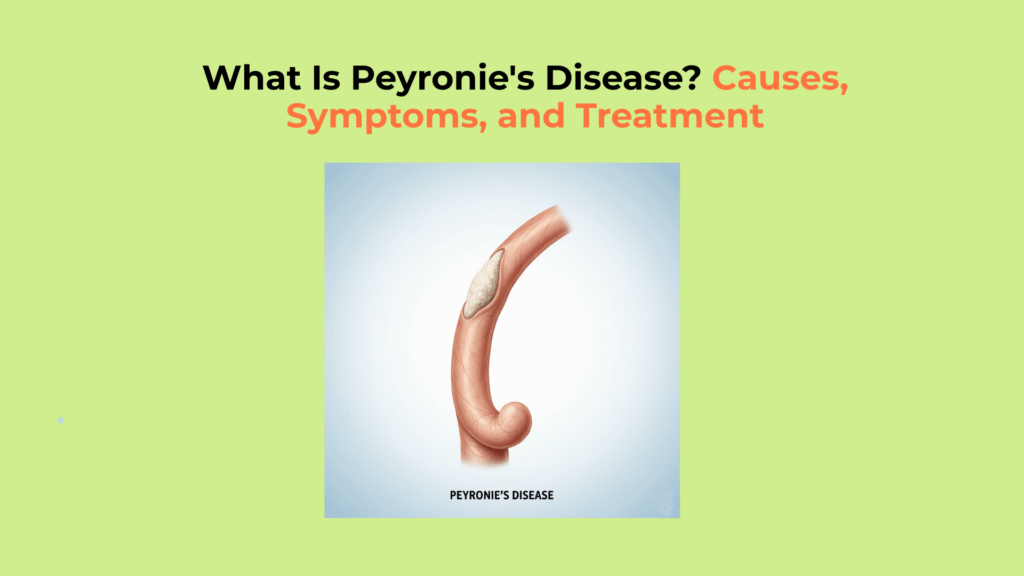
Peyronie’s disease is an acquired connective tissue disorder where fibrous scar tissue (plaque) forms within the tunica albuginea of the penile anatomy, causing erections to become curved and often painful.
This acquired penile curvature develops later in life and is not a congenital condition, nor is it cancerous. While the resulting bend in the penis can cause significant functional and psychological distress, Peyronie’s disease is highly treatable.
This guide provides a clinical, evidence-based framework to understand what Peyronie’s disease is, its causes, how to identify its symptoms by its two phases, and the most effective modern treatment options. Peyronie’s disease should not be confused with congenital chordee, which is present at birth rather than acquired.
Key Takeaways on Peyronie’s Disease
- What it is: Peyronie’s Disease is a progressive, non-cancerous disorder causing an acquired penile curvature due to scar tissue (plaque).
- Primary Cause: A disordered wound healing response following microtrauma (minor injury) to the penis, often during vigorous sex.
- Core Symptoms: Painful erections, a palpable hard lump (plaque on penis), and significant curvature (bend) during an erection.
- Treatment Focus: Treatment for Peyronie’s Disease aims to stabilize the curve and restore functional sex via injections (Collagenase) or surgery.
What Causes Peyronie’s Disease to Develop?
The causes of Peyronie’s disease center on an abnormal wound healing response to microtrauma in the tunica albuginea, the sheath around the erectile tissues, which results in the deposition of inelastic scar tissue (plaque).
How Microtrauma Leads to Peyronie’s Plaque Formation
Peyronie’s disease is most often triggered when microtrauma—such as excessive bending or buckling of the penis during sexual activity—damages the tunica albuginea, causing a disordered healing response (NIDDK). The tunica albuginea is the strong, elastic sheath of tissue that surrounds the corpora cavernosa (the main erectile chambers).
Instead of repairing the damage with flexible tissue, the body overproduces Type I collagen, forming a dense, localized fibrous plaque. When the penis becomes erect, the healthy surrounding tissue expands, but the rigid Peyronie’s plaque cannot stretch, which pulls the shaft into a curve or bend (PubMed – Pathophysiology).
Why Certain Individuals Are Prone to Peyronie’s Disease
Certain individuals are prone to Peyronie’s disease due to risk factors like a genetic predisposition for abnormal healing, associated connective tissue disorders like Dupuytren’s contracture, and underlying health conditions such as diabetes.
Peyronie’s disease is most common in men aged 50-70 and has a strong association with Dupuytren’s contracture (a similar scarring condition in the hand), according to the Mayo Clinic.
- Connective Tissue Disorders: Association with Dupuytren’s contracture and plantar fasciitis.
- Age: Most common in men aged 50–70.
- Underlying Health: Conditions like diabetes and Erectile Dysfunction (ED) increase susceptibility.
- Genetics: A family history suggests a genetic predisposition.
How to Identify the Symptoms and Stages of Peyronie’s Disease
The symptoms of Peyronie’s Disease are identified by a characteristic set of physical changes to the penis that evolve over two distinct phases: an acute phase and a chronic phase. Recognizing which phase you are in is crucial for determining the right treatment (Urology Health).
You can visually assess curvature using our Curvature & Lesion Clarity Tool to better understand the shape, angle, and plaque development before visiting a urologist.
The Two Phases of Peyronie’s Disease
Peyronie’s disease progresses in two distinct phases: an initial acute phase where inflammation is active and the curvature is worsening, followed by a stable chronic phase where the pain resolves but the plaque and curvature are fixed.
| Phase | Typical Duration | Primary Status | Key Symptoms & Actionable Takeaway |
|---|---|---|---|
| Acute Phase | 5 to 18 months | Active Plaque Formation (Curve Worsening) | Painful erections is common. The curve is actively changing. Action: Seek treatment immediately; non-surgical options are most effective now. |
| Chronic Phase | After 12–18 months | Stable/Calcified Plaque (Curve Fixed) | Pain usually resolves. The curve is stable. Action: Surgical options are now considered the most definitive treatment. |
Source: Adapted from Urology Health Foundation.
Core Symptoms of Peyronie’s Disease
The core symptoms of Peyronie’s Disease include a palpable hard lump (plaque on penis) under the skin, a noticeable penile curvature during erection, and, especially in the acute phase, painful erections.
- Palpable Lumps: The scar tissue (plaque) can be felt as a hard lump or band under the skin.
- Penile Curvature/Bend: The bend can be upward, downward, or sideways, most visible during an erection.
- Erectile Pain: Pain during erections (occurs mainly in the acute phase).
- Loss of Length/Girth: The penis may appear shorter when erect, or develop indentations, sometimes creating an “hourglass” or “bottleneck” deformity.
How Is Peyronie’s Disease Treated?
Treatment for Peyronie’s Disease is guided by the disease stage and the resulting functional impairment, with non-surgical options (injections, traction) used in the acute phase and surgical correction reserved for the stable chronic phase. Consulting a urologist is the first step in creating a tailored plan.
Non-Surgical Treatments for Active Disease (Acute Phase)
Non-surgical treatment for Peyronie’s disease in the acute phase aims to reduce pain, minimize curvature, and stabilize the plaque using injections or traction devices.
- Penile Traction Therapy (PTT): This involves wearing a stretching device on the penis for set periods daily to counteract the curve and limit length loss.
- Injectable Therapy (CCH): The primary FDA-approved treatment is Collagenase Clostridium Histolyticum (CCH) (brand name Xiaflex). This is an enzyme injected directly into the plaque to break down the collagen that makes up the scar tissue, thereby reducing the bend.
Surgical Correction for Stable Disease (Chronic Phase)
Surgical treatment for Peyronie’s disease is the most definitive option for the chronic phase and is recommended for men with a stable curvature that prevents sexual function (Urology Health – Surgical Options). Orthoplasty is the general medical term for these straightening procedures.
- Plication (Shortening): This involves placing permanent sutures on the long (convex) side of the curve to shorten it and balance the curvature. The Nesbit procedure is a common example of this. The drawback is that it results in minor penile length loss.
- Grafting (Lengthening): This involves cutting the plaque and patching the gap with a tissue graft to lengthen the constricted (concave) side. This is typically used for severe bends.
- Penile Prosthesis Implantation: This is the best option for men with both severe curvature and significant pre-existing Erectile Dysfunction (ED), as it corrects both issues simultaneously.
Men experiencing both curvature and erectile issues may benefit from combining surgery with the Erectile Dysfunction Recovery Blueprint to support post-surgical recovery and improve erectile function.
Key Takeaways for Managing Peyronie’s Disease
Managing Peyronie’s disease effectively requires consulting a urologist immediately to get an accurate diagnosis, understanding that while the scar tissue is permanent, treatment is highly successful at restoring sexual function and resolving pain for most men.
With modern treatments, a diagnosis of Peyronie’s disease is not the end of a healthy sex life, but the beginning of a manageable treatment plan.
Glossary of Clinical Terms
To ensure full clarity, this glossary defines the key clinical and scientific terms used throughout this guide on Peyronie’s disease.
| Term | Definition |
|---|---|
| Peyronie’s Disease | An acquired condition where fibrous scar tissue (plaque) forms in the tunica albuginea of the penis, causing curvature and pain. |
| Tunica Albuginea | The strong, elastic, fibrous sheath of tissue that surrounds the erectile chambers (corpora cavernosa). |
| Plaque | The hard, inelastic, palpable lump of scar tissue (fibrosis) that is the hallmark of Peyronie’s disease. |
| Acute Phase | The initial, inflammatory stage of the disease (lasting 5-18 months) characterized by pain and a changing or worsening curvature. |
| Chronic Phase | The later, stable stage of the disease where pain typically resolves, but the plaque and curvature are fixed. |
| Collagenase (CCH) | An enzyme (brand name Xiaflex) that is injected into the plaque to break down the excess collagen and reduce curvature. |
| Orthoplasty | The general medical term for any surgical procedure that straightens the penis. |
| Plication | A surgical technique (e.g., Nesbit procedure) that shortens the longer side of the penis to straighten the curve. |
References
- Mayo Clinic – Peyronie’s Disease: Symptoms and Causes
- Urology Care Foundation – Peyronie’s Disease Overview & Phases
- Urology Care Foundation – Surgical Options for Peyronie’s Disease
- Official Xiaflex® (Collagenase Clostridium Histolyticum) Treatment Information
- American Urological Association (AUA) – Peyronie’s Disease Clinical Practice Guideline
- PubMed – Pathophysiology and Treatment Advances in Peyronie’s Disease (2020)
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Peyronie’s Disease
- Medscape – Peyronie’s Disease Overview (Clinical Summary)




5 Responses