What Is Phimosis? A Guide to Causes, Symptoms, and Treatment
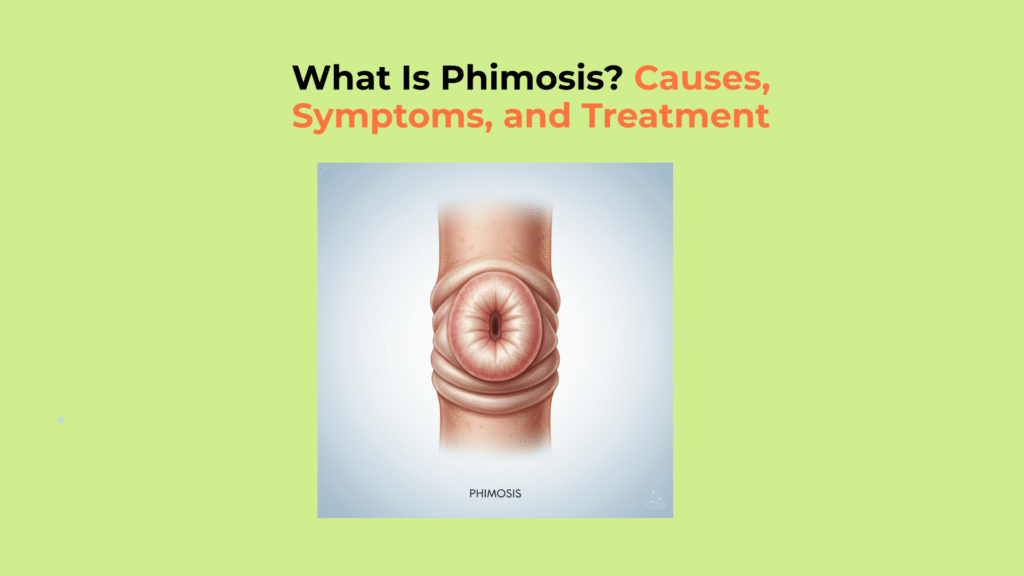
Phimosis is the medical term for the inability to retract the foreskin (prepuce) completely over the glans (head of the penis)—a part of the penile anatomy responsible for protection and sexual sensitivity.
This condition is normal in infants but becomes a medical issue if it persists into adulthood due to scarring. The stricture of the preputial opening prevents full exposure of the glans, compromising both sexual function and routine hygiene. While a tight foreskin is common during early development, persistence into adulthood can lead to chronic inflammation and serious complications.
This guide provides a clinical, evidence-based framework to understand what phimosis is, how to differentiate the normal physiologic type from the problematic pathologic type, and the most effective treatment for phimosis options.
Key Takeaways on Phimosis
- What it is: Phimosis is the stricture of the preputial opening, preventing full foreskin retraction.
- The Etiological Divide: It is considered problematic only if it is pathologic (scarred), often due to Lichen Sclerosus (BXO) or chronic infection.
- Primary Task Failure: The condition causes failure in genital hygiene and painful or impossible sexual function.
- Treatment Strategy: Initial action is topical corticosteroid therapy. Surgery is the definitive cure for scarring or treatment failure.
What Causes Phimosis to Develop and Become Problematic?
The primary clinical task in managing phimosis is distinguishing physiologic phimosis (a normal developmental tightness in children) from pathologic phimosis (an acquired, problematic condition caused by scarring). The underlying cause dictates the necessary course of action, which is why accurate diagnosis is crucial.
How Do Physiologic and Pathologic Phimosis Differ Clinically?
Physiologic phimosis is the normal, developmental non-retractability of the foreskin in infants, which resolves spontaneously, while pathologic phimosis is an acquired, non-resolving condition caused by a rigid scar tissue ring.
| Feature | Physiologic Phimosis (Normal Childhood State) | Pathologic Phimosis (Acquired/Scarred Disease) |
|---|---|---|
| Etiology | Natural adhesion/developmental delay; resolves spontaneously. | Fibrosis (scarring) due to chronic inflammation or injury. |
| Appearance | Foreskin tip is supple, moist, and unscarred. | Foreskin tip has a white, rigid, inelastic, or fibrotic ring. |
| Intervention | None; forcible retraction is contraindicated (causes scarring). | Requires active intervention (steroid cream or surgery). |
At birth, the inability to retract the foreskin is a normal state. The American Academy of Pediatrics (AAP) indicates that by age 3, approximately 90% of foreskins are naturally retractable. By ages 16–17, only about 1% of males are estimated to still have phimosis (Source: AAP). Therefore, in adolescents and adults, the condition is far more likely to be the pathologic phimosis type.
Which Underlying Conditions Increase the Risk of Pathologic Phimosis?
The primary risk factor for pathologic phimosis in adults is Lichen Sclerosus (BXO), a chronic skin condition that creates scarring, often exacerbated by recurrent balanitis from poor hygiene or uncontrolled Diabetes Mellitus. These acquired causes create the characteristic rigid, white ring around the preputial opening that defines problematic phimosis.
- Lichen Sclerosus (BXO): This is the most common etiology of acquired phimosis in men. It is a chronic dermatosis that produces a white, inelastic scar tissue ring at the tip of the foreskin. This progressive scarring makes normal retraction impossible (Source: NCBI).
- Diabetes Mellitus: Uncontrolled hyperglycemia leads to glucose in the urine, which promotes Candida (yeast) growth. This often results in recurrent balanoposthitis (inflammation of the glans and foreskin), which in turn causes chronic inflammation and subsequent fibrosis (scarring).
- Poor Hygiene: Inadequate cleansing of the sub-preputial space leads to chronic balanitis (inflammation of the glans), a frequent cause of scarring that restricts the preputial opening and results in pathologic phimosis.
What Are the Key Symptoms and Functional Effects of Phimosis?
The key “symptoms of phimosis” are primarily functional, including painful erections (dyspareunia), “ballooning” of the foreskin during urination, and an inability to maintain hygiene, which leads to recurrent infections. These functional issues signal a need for clinical evaluation.
- Impaired Sexual Function (Dyspareunia): Painful intercourse occurs because the restricted preputial opening stretches painfully during erection, causing pain, tearing, or splitting of the foreskin tissue. Dyspareunia is defined as difficult or painful sexual intercourse.
- Impaired Micturition (Urination): The tight foreskin orifice restricts urine flow, causing the foreskin to “balloon” or bulge (preputial distention) during urination, often leading to a weak or spraying stream.
- Hygiene Deficit: The inability to retract the foreskin prevents proper cleansing of the sub-preputial space. This causes the chronic accumulation of smegma (cellular debris) and fosters infection and balanitis.
Why Is Paraphimosis a High-Risk Complication of Phimosis?
Paraphimosis is a urological emergency and a high-risk complication of phimosis, where the tight foreskin is retracted behind the glans and becomes trapped, acting as a tourniquet that cuts off blood flow.
This forms a tourniquet-like constriction, causing rapid edema and swelling of the glans, which potentially leads to ischemia and tissue necrosis if not immediately resolved. Paraphimosis requires immediate medical attention to prevent tissue death and is always treated as an acute emergency (Source: Mayo Clinic).
How Is Symptomatic Phimosis Effectively Treated?
Symptomatic phimosis is effectively treated using a tiered management strategy, starting with a non-surgical, first-line “treatment for phimosis” using topical corticosteroid creams, with surgery reserved for cases that fail therapy or involve severe scarring.
What is the First-Line Non-Surgical Treatment for Phimosis?
The first-line non-surgical “treatment for phimosis” is a 4- to 8-week course of a high-potency topical steroid cream combined with gentle, manual stretching.
- Topical Steroid Therapy: Apply a high-potency corticosteroid (e.g., Clobetasol Propionate 0.05%) directly to the fibrotic ring twice daily for 4–8 weeks. This action reduces inflammation and promotes tissue elasticity.
- Guided Stretching: Initiate gentle manual stretching concurrent with cream application, only to the point of light tension, to promote tissue elasticity without causing tears.
This conservative approach is highly effective, with success rates reported between 70-90% in clinical studies, often resolving the inability to retract the foreskin (Source: NCBI PMC).
When Is Surgery Necessary to Correct Phimosis?
Surgical “treatment for phimosis” is necessary following the failure of conservative steroid cream therapy, for moderate-to-severe scarring caused by Lichen Sclerosus (BXO), or as an emergency procedure for paraphimosis.
- Circumcision: The “gold standard” and definitive solution. It involves the complete surgical excision of the prepuce, permanently resolving the condition and all associated risks.
- Preputioplasty: A foreskin-preserving option. The tight ring is widened through controlled longitudinal incisions and transverse suturing. This technique maintains the foreskin while addressing the stricture (Source: Urology Health). The American Urological Association (AUA) supports both methods as effective treatment options.
How Does Treating Phimosis Affect the Long-Term Prognosis?
The long-term prognosis for treated phimosis is excellent, as both steroid cream therapy and surgical correction are highly effective at restoring normal foreskin retractability, eliminating pain, and resolving hygiene issues.
Because phimosis is a highly treatable condition, most patients achieve a complete resolution of their functional symptoms of phimosis. This outcome reinforces that seeking timely intervention is key. Consulting a urologist for a definitive diagnosis is the most important step toward resolving this common and treatable condition.
Glossary of Clinical Terms
To ensure full clarity, this glossary defines the key clinical and scientific terms used throughout this guide on phimosis.
| Term | Definition |
|---|---|
| Phimosis | A condition where the foreskin is too tight to be retracted back over the glans (head of the penis). |
| Pathologic Phimosis | Phimosis caused by scarring, inflammation, or a skin condition, as opposed to normal developmental tightness. |
| Lichen Sclerosus (BXO) | A chronic, inflammatory skin condition that is the most common cause of pathologic phimosis in adults. |
| Paraphimosis | A urological emergency where the retracted foreskin becomes trapped behind the glans, cutting off blood flow. |
| Clobetasol Propionate | A high-potency topical corticosteroid cream used as a first-line non-surgical treatment for phimosis. |
| Preputioplasty | A foreskin-preserving surgical procedure that widens the tight foreskin opening. |
| Balanitis | Inflammation, redness, and swelling of the glans (head of the penis) only. |
| Balanoposthitis | Inflammation that involves both the glans (head of the penis) and the foreskin. |




2 Responses