Venous-Leak Penis: Causes of Poor Erection Maintenance (A Diagnostic Guide)
Listen to the Article
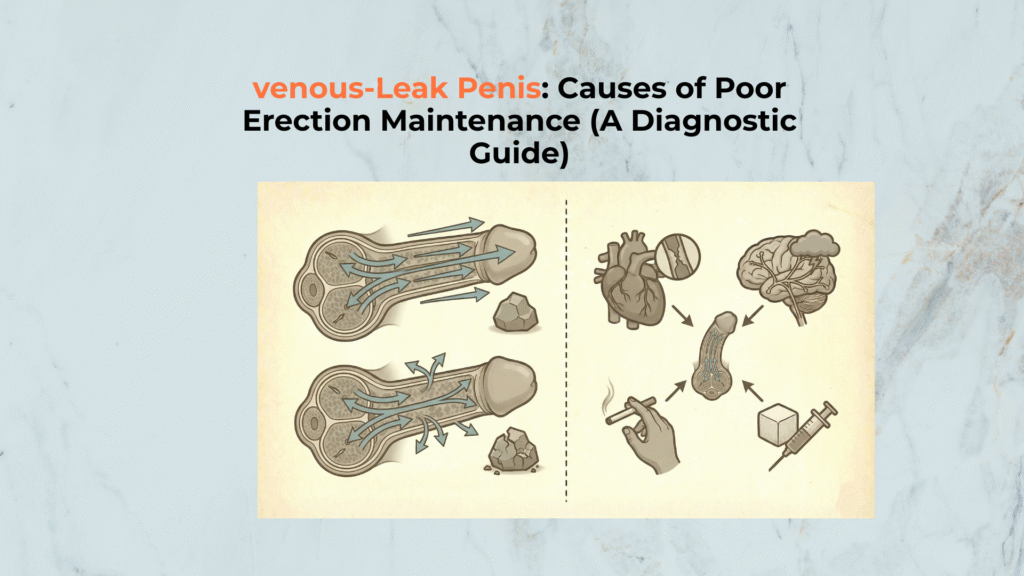
The Venous-Leak Penis, clinically known as Corporal Veno-Occlusive Dysfunction (CVOD), is a pathological condition defined by the inability to trap blood within the Corpora Cavernosa.
This results in a rapid loss of erection firmness. This failure of the hydraulic mechanism is not merely an anatomical defect but often a systemic marker of Endothelial Dysfunction.
Important Medical Disclaimer
This guide is for informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for any questions regarding your health or erectile function.
Why Is the Venous-Leak Penis a Primary Indicator of Underlying Vascular Disease?
The Venous-Leak Penis is a primary indicator of underlying vascular disease because the mechanism of its failure (CVOD) shares the same root cause as systemic cardiovascular conditions: Endothelial Dysfunction [2].
How Is the Venous-Leak Penis Clinically Defined?
The Venous-Leak Penis is clinically defined by its failure to maintain rigidity, which results from the Corpora Cavernosa losing the ability to compress outflow veins fully.
CVOD is a pressure-trapping failure inside the erectile chambers, so review the corpora cavernosa to anchor what must stay pressurized to maintain firmness.
This inability to maintain intracavernosal pressure, despite adequate arterial inflow, leads to maintenance failure.
Clinical data from Montorsi [4] and Ma [6] defines abnormal maintenance as a pressure drop of >50 mmHg within 30 seconds.
In summary: The Venous-Leak Penis → fails to maintain intracavernosal pressure → leading to rapid detumescence.
| Vascular Status | Pathological Mechanism | EHS Symptom |
|---|---|---|
| Arterial Insufficiency | Insufficient blood inflow. | Inability to achieve EHS 3/4. |
| Venous-Leak (CVOD) | Failure to trap blood. | Achieve EHS 3/4 briefly, then rapid detumescence. |
| Psychogenic ED | Neurological interference. | Variable quality; often resolves with distraction. |
How Does the Venous-Leak Penis Indicate Systemic Cardiovascular Risk?
The Venous-Leak Penis indicates systemic cardiovascular risk because the underlying Endothelial Dysfunction that causes the leak often afflicts the coronary arteries simultaneously [2].
Penile arteries are smaller and show damage significantly earlier than coronary arteries, acting as a “canary in the coal mine.”
Logic: Endothelial dysfunction → degrades vascular integrity system-wide → positioning CVOD as a predictor of cardiovascular events.
For more on how vascular health shapes anatomy, review the Penis Shape Overview.
Systemic Risks Associated with CVOD
- Endothelial Dysfunction: Shared damage to blood vessel lining.
- Shared Risk Factors: Smoking, Diabetes, and Hypertension accelerate both conditions.
- Vascular Bed Size: Penile arteries are smaller, showing damage earlier than coronary arteries.
What Pathophysiology Underlies Venous Occlusion Failure in the Venous-Leak Penis?
Venous Occlusion failure in the Venous-Leak Penis is primarily caused by structural damage to the Cavernosal Smooth Muscle and inelasticity of the Tunica Albuginea [3].
The “seal” that enables venous compression is structural, and the best single map is the tunica albuginea role because CVOD happens when this capsule can’t support occlusion.
Which Anatomical Structures Govern Venous Leakage in the Venous-Leak Penis?
Anatomical structures governing venous leakage in the Venous-Leak Penis are the Tunica Albuginea (outer sheath) and the Emissary Veins (outflow), whose failure prevents adequate pressure retention [5].
Damage to subtunical smooth muscle prevents the compression of veins against the tunica. Nehra [3] established that smooth muscle content correlates directly with leakage control.
Mechanism: Damage to the subtunical smooth muscle fibers → prevents compression of Emissary Veins → allowing blood to leak out.
Venous leak is defined by persistent outflow, so connect the mechanism to the actual drainage anatomy in penile veins to understand where “escape routes” remain open.
| Structural Component | Role in Rigidity | Failure in Venous-Leak Penis |
|---|---|---|
| Tunica Albuginea | Pressure capsule. | Often thinned or inelastic. |
| Cavernosal Smooth Muscle | Traps blood. | Fibrosis/Failure to Relax seals veins poorly [3]. |
| Emissary Veins | Outflow vessels. | Incomplete Compression allowing leak. |
How Do Lifestyle Factors Accelerate Damage to the Venous-Leak Penis Mechanism?
Lifestyle factors accelerate damage to the Venous-Leak Penis mechanism through chronic systemic stress (e.g., smoking, diabetes), which causes widespread Endothelial Dysfunction and tissue fibrosis.
Conditions like diabetes and hypertension damage the integrity of the vascular system, as noted in AUA Guidelines [1].
Etiology: Chronic poor lifestyle choices → lead to widespread endothelial damage → accelerating the progression of venous leakage.
If the venous-leak pattern is part of a curvature/fibrosis phenotype, route readers to Peyronie’s disease because tunica remodeling can intersect with occlusion mechanics.
Etiology Focus: Lifestyle Acceleration of Venous-Leak Penis
- Diabetes: Damages smooth muscle cells (SMCs) in the Corpora.
- Hypertension: High pressure degrades vascular integrity.
- Smoking: Severe vasoconstriction impairs relaxation needed for sealing.
How Are Venous-Leak Penis Symptoms Accurately Diagnosed?
Venous-Leak Penis symptoms are accurately diagnosed by combining patient self-screening criteria (rapid detumescence) with specialized clinical tests like Dynamic Infusion Cavernosometry (DICC).
Your diagnostic logic compares inflow vs outflow, and the cleanest pathway-level overview is the vascular pathway which frames why good inflow can still end in rapid detumescence.
How to Perform Self-Screening for the Venous-Leak Penis
Self-screening for the Venous-Leak Penis requires focusing on the Detumescence Rate—the speed at which firmness is lost—as the primary indicator of CVOD. Erection is achieved but lost rapidly during movement.
The AUA Guidelines [1] suggest using validated questionnaires (SHIM/IIEF) for assessment.
Indicator: Rapid loss of erection firmness → correlates strongly with Venous-Leak pathology → serving as the primary self-screening indicator.
Self-Screening Checklist for the Venous-Leak Penis
- ✓ Tumescence Rate: Erection achieved quickly, but firmness drops rapidly.
- ✓ Maintenance Failure: Difficulty keeping an erection during position changes.
- ✓ Morning Erection Quality: Reduced firmness or absence.
Which Clinical Tests Confirm the Venous-Leak Penis Diagnosis?
Clinical tests confirm the Venous-Leak Penis diagnosis through vascular assessment, primarily utilizing the Dynamic Infusion Cavernosometry (DICC) to measure outflow integrity [4, 6].
This test diagnoses the specific flow rate required to maintain erection. Montorsi [4] and Ma [6] define CVOD as a flow-to-maintain of >10 mL/min.
Confirmation: The specialized DICC test → measures flow-to-maintain → quantitatively diagnosing the degree of venous leakage.
- Doppler Ultrasound: Assesses inflow vs. outflow signatures.
- DICC (Cavernosometry): Measures pressure necessary to prevent venous outflow.
How Do Medical and Surgical Techniques Treat the Venous-Leak Penis?
Medical and surgical techniques treat the Venous-Leak Penis by attempting to maximize arterial inflow to overpower the leak (medical) or by surgically ligating the failed outflow vessels (surgical).
Which Non-Surgical Treatments Offer Efficacy for the Venous-Leak Penis?
Non-surgical treatments for the Venous-Leak Penis, such as PDE5 Inhibitors, offer efficacy by boosting arterial inflow, which helps temporarily compensate for the outflow loss [8].
These are effective for mild leaks or combined arterial issues but often fail in severe CVOD. CUA Guidelines [8] identify PDE5i as the first-line attempt.
Mechanism: PDE5 inhibitors → maximize arterial inflow → attempting to overpower the vein leak via high pressure.
| Treatment Modality | Functional Goal | Applicability |
|---|---|---|
| PDE5 Inhibitors | Maximize arterial inflow. | Effective for mild leaks/mixed ED [8]. |
| VED (Vacuum Device) | Physical occlusion via ring. | Effective for immediate function; non-curative. |
| Lifestyle Changes | Improve endothelial health. | Essential foundation for all treatments. |
How Are Surgical Interventions Used to Cure the Venous-Leak Penis?
Surgical interventions are used to address the Venous-Leak Penis by physically sealing the defective outflow vessels, although this is generally considered a last-resort treatment [7].
The procedure, Dorsal Vein Ligation, involves tying off outflow vessels. Popken [7] notes that success rates often decline over time.
Strategy: Surgical ligation → attempts to tie off leaking veins → restoring pressure retention within the corpora.
Surgical Protocol Checklist
- ! Last Resort: Surgery is typically reserved for cases unresponsive to medication.
- ! Procedure: Dorsal Vein Ligation (tying off outflow vessels).
- ! Prognosis: Success rates vary; often requires continued lifestyle management.
Conclusion: What Final Action Protocol Ensures Optimal Management of the Venous-Leak Penis?
The final action protocol ensuring optimal management of the Venous-Leak Penis synthesizes the necessity for definitive diagnosis, strict lifestyle modification, and immediate cardiovascular health assessment. CVOD serves as a “Vascular Alarm Bell” that must not be ignored.
Key Pathophysiological Takeaways
- Failure to Trap Blood: Mechanism relies on inadequate Venous Occlusion.
- Primary Vascular Etiology: Root cause is typically Endothelial Dysfunction.
- Predictor of Systemic Risk: The condition indicates potential for future cardiovascular events [2].