What Is Penile Chancroid? A Guide to Causes, Symptoms, and Treatment
Chancroid is a bacterial sexually transmitted infection (STI) caused by Haemophilus ducreyi that results in painful genital ulcers known as “soft chancres” (CDC STD Facts).
Chancroid is frequently confused with other STIs that cause genital sores, but it has distinct features. This infection is highly contagious and, importantly, is fully curable with the correct antibiotics.
This guide provides a clinical explanation of what penile chancroid is. We will cover its cause, how to identify its symptoms, and the definitive treatment options.
Key Takeaways on Penile Chancroid
- What it is: Chancroid is an STI caused by the bacterium Haemophilus ducreyi. It results in painful, soft ulcers on the genitals.
- Primary Cause: The bacterium Haemophilus ducreyi is transmitted through sexual contact or non-sexual contact with an infected open sore.
- Core Symptoms: The main symptoms are painful genital ulcers and often swollen, tender lymph nodes in the groin (buboes).
- Treatment: Chancroid is curable with a single-dose or short course of antibiotics (e.g., Azithromycin or Ceftriaxone).
What Causes Chancroid on the Penis?
Chancroid on the penis is caused by a specific bacterium, Haemophilus ducreyi, which is transmitted through sexual contact and invades the skin through micro-abrasions (StatPearls – Chancroid).
How the Haemophilus ducreyi Bacterium Causes Chancroid
The Haemophilus ducreyi bacterium causes chancroid by entering microscopic breaks in the skin during sexual contact, then releasing toxins that destroy skin tissue, leading to an open ulcer.
The incubation period is typically 4 to 10 days after exposure. Chancroid is rare in the United States but is endemic in many tropical and developing regions, such as parts of Africa and Asia (WHO).
Risk Factors and Transmission of Chancroid
The primary risk factor for chancroid is sexual contact with an infected individual, with transmission being significantly facilitated by the presence of open sores, being uncircumcised, and co-infection with HIV.
- Sexual Contact: Spreads through vaginal, anal, or oral sex with an infected person.
- Skin-to-Skin Contact: The highly infectious fluid (pus) from the sore can transmit the bacteria through non-sexual physical contact.
- Uncircumcision: Uncircumcised men have a higher risk of acquiring chancroid, as the area under the foreskin can trap the bacteria.
- HIV Risk: The presence of chancroid ulcers significantly increases the risk of acquiring and transmitting HIV by providing an easy portal of entry for the virus (PMC – HIV & Genital Ulcers).
What Are the Key Symptoms of Penile Chancroid?
The key symptoms of penile chancroid are the development of one or more “soft chancres”—painful, pus-filled genital ulcers—often followed by painfully swollen lymph nodes in the groin known as buboes (DermNet NZ).
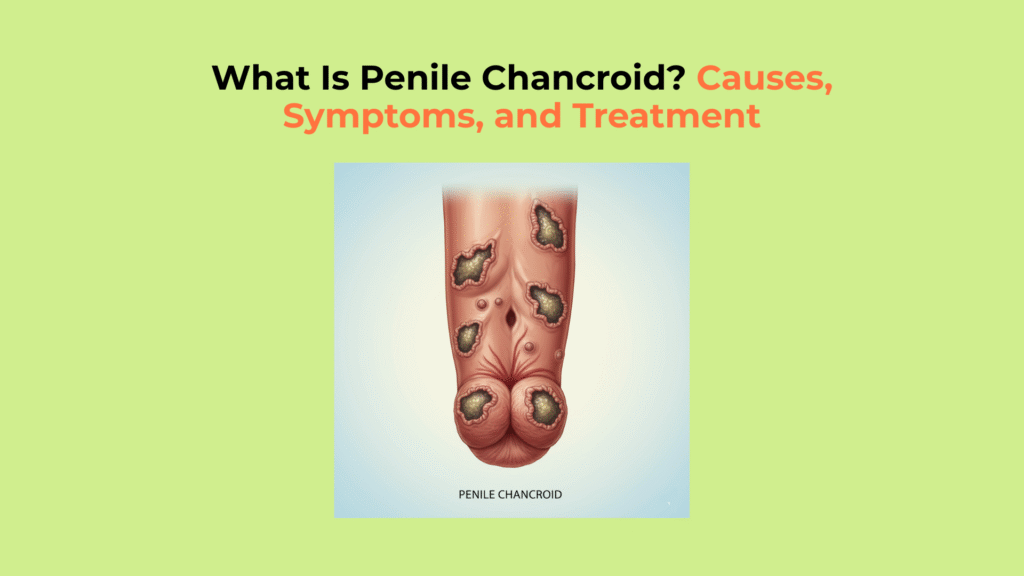
How to Identify a Chancroid Ulcer (The Soft Chancre)
A chancroid ulcer is identified by its key characteristics: it is very painful, has soft, ragged edges, and a greyish-yellow base, which distinguishes it from the painless “hard chancre” of syphilis.
Symptoms usually appear 4 to 10 days after exposure. The infection begins as a small, tender red bump that quickly becomes a pus-filled sore (pustule) and then ruptures into an open ulcer.
The ulcer’s characteristics include:
- Pain: The ulcer is characteristically very painful. This is the primary differentiator from the painless “hard chancre” of primary syphilis.
- Margins: It has soft, irregular, or ragged edges (undermined borders).
- Base: The base is usually covered with a gray or yellowish pus (purulent exudate) and bleeds easily when touched.
- Location: On the penis, they commonly form on the foreskin, coronal groove (behind the glans), or penile shaft.
Recognizing Associated Chancroid Symptoms
Associated chancroid symptoms include the development of buboes (swollen lymph nodes) in about 50% of cases, pain during urination, and potential scarring or phimosis in uncircumcised men (Medscape – Chancroid Overview). Buboes are painfully swollen lymph nodes in the groin.
- Buboes: In about 50% of infected men, the lymph nodes in the groin become painfully swollen, forming a pus-filled abscess called a bubo, which can rupture through the skin.
- Dysuria: Painful urination, especially if the ulcer is near the urethral opening.
- Complications in Uncircumcised Males: Untreated ulcers can lead to significant scarring and tissue destruction, potentially causing phimosis (inability to retract the foreskin).
How Do Doctors Diagnose Chancroid?
Doctors diagnose chancroid primarily through a clinical evaluation of the painful ulcers, combined with tests to definitively rule out other, more common STIs like syphilis and herpes (StatPearls – Genital Ulcers).
A definitive diagnosis by culturing H. ducreyi is difficult. This process is not widely available and requires special laboratory media to grow the bacteria.
Therefore, a probable diagnosis is often made based on these 4 factors:
- One or more painful genital ulcers are present.
- The patient tests negative for syphilis (via darkfield microscopy or serological tests).
- The patient tests negative for herpes simplex virus (HSV) via PCR or culture from the ulcer.
- The clinical appearance of the ulcers is consistent with chancroid (soft chancre, buboes).
(Source: CDC Treatment Guidelines)
What Is the Treatment for Chancroid?
The treatment for chancroid is highly effective and consists of a specific course of antibiotics, with the CDC recommending a single-dose regimen of Azithromycin or Ceftriaxone as the preferred, most reliable option (CDC Treatment Guidelines).
How Antibiotics Cure Chancroid
Antibiotics cure chancroid by eliminating the H. ducreyi bacteria, with the CDC-recommended single-dose regimens being the most effective treatment for ensuring patient compliance (Merck Manual Pro).
Single-Dose Regimens (Preferred):
- Azithromycin: 1 gram taken orally in a single dose.
- Ceftriaxone: 250 mg given as an intramuscular (IM) injection in a single dose.
Multi-Day Regimens (Alternatives):
- Ciprofloxacin: 500 mg orally, twice a day for 3 days.
- Erythromycin: 500 mg orally, three times a day for 7 days (CDC Treatment Guidelines, 2021).
Key Steps for Successful Chancroid Management
Successful chancroid management requires diligent medical follow-up, potential drainage of buboes, and the immediate treatment of all recent sexual partners to prevent reinfection.
How Can Chancroid Be Prevented?
Chancroid can be prevented by practicing safe sex, including the consistent use of condoms, and by limiting the number of sexual partners, which reduces the risk of exposure to Haemophilus ducreyi (CDC – STD Prevention).
Chancroid Prevention Checklist
The most important action is to see a healthcare professional immediately for any painful genital sore. This ensures a correct diagnosis to differentiate it from syphilis or herpes and allows for the correct antibiotic treatment to begin.
Understanding that chancroid is a common, curable condition is the first step toward treating it quickly and preventing its spread. At Factbasedurology, we believe that clear, non-judgmental information about STIs is the best way to empower individuals to protect their health and the health of their partners.
Glossary of Clinical Terms
To ensure full clarity, this glossary defines the key clinical and scientific terms used throughout this guide on chancroid.
| Term | Definition |
|---|---|
| Chancroid | A sexually transmitted infection (STI) caused by the bacterium Haemophilus ducreyi, characterized by painful genital ulcers. |
| Haemophilus ducreyi | The specific bacterium that causes chancroid. |
| Soft Chancre | The painful, soft-edged ulcer characteristic of chancroid, differentiating it from the “hard chancre” of syphilis. |
| Bubo (Buboes) | A painful, swollen, and abscessed lymph node in the groin, a common complication of chancroid. |
| Syphilis | A different STI that, in its primary stage, produces a painless ulcer called a “hard chancre.” |
| Phimosis | A condition in uncircumcised males where the foreskin is too tight to be retracted back over the glans, sometimes a complication of chancroid scarring. |




One Response