What Is a Buried Penis? A Guide to Causes, Symptoms, and Treatment
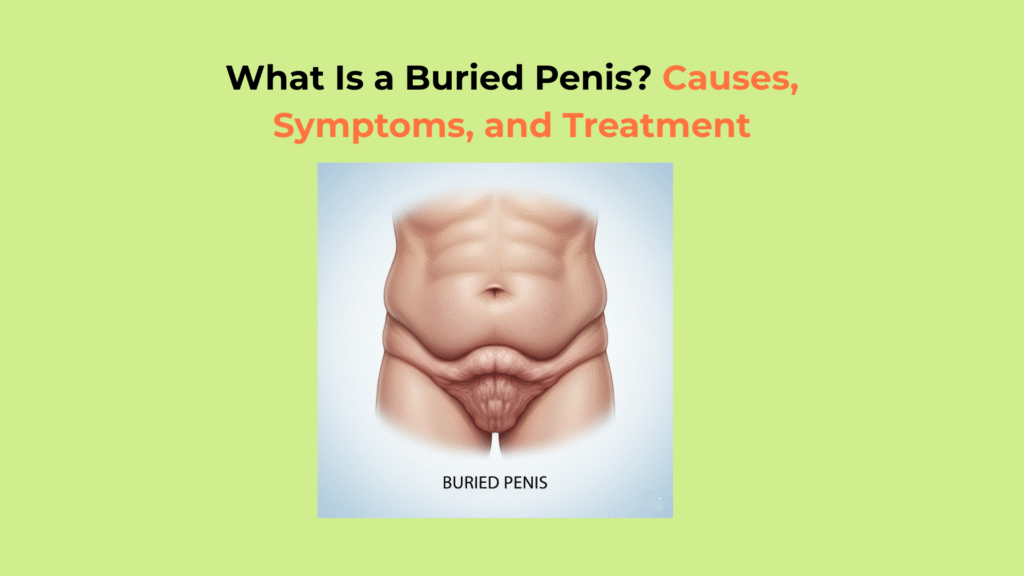
A buried penis is a condition where a normal-sized penis is hidden underneath the skin of the abdomen, scrotum, or thighs, a problem that is most often acquired in adults due to obesity but is highly treatable.
This condition is not the same as a micropenis (an anatomically small penis), and the physical and psychological distress it causes is real, significant, and treatable. A buried penis is characterized by a penis of normal size (Entity) that is concealed (Action) by surrounding skin and fat (Result).
This guide provides a clinical explanation of what a buried penis is. We will cover its causes, the functional symptoms it creates, and the effective surgical and non-surgical treatments.
Key Takeaways on Buried Penis
- What it is: A buried penis is a penis of normal size that is concealed by surrounding skin and fat, making it appear very small or invisible.
- Primary Cause: In adults, the most common cause of a buried penis is obesity, where a large suprapubic fat pad (mons pubis) covers the penis. In children, it is often a congenital issue with the ligaments supporting the penis.
- Core Symptoms: A buried penis causes functional problems, including difficulty with urination (spraying, dribbling), poor hygiene, recurrent skin infections, and psychological distress.
- Treatment Focus: Treatment for a buried penis aims to “unbury” the penis. This often requires surgical procedures to remove excess fat and skin (like an escutcheonectomy) and secure the penis in its proper position.
What Causes a Buried Penis?
The “causes of a buried penis” are categorized into two distinct types: acquired (developing in adulthood, most often from obesity) and congenital (present at birth due to abnormal ligament attachments).
How an Acquired Buried Penis Develops in Adults
An acquired buried penis develops in adults most frequently due to morbid obesity, where a large pad of abdominal fat (pannus) hangs over and envelops the penis (AUA – Diagnosis & Management). This large apron of fat and skin in the suprapubic area, known medically as the pannus or escutcheon, can completely cover the genitals, trapping the penis underneath.
Other acquired causes include:
- Genital Lymphedema: Severe swelling of the scrotum and genital area, which can be caused by infection, radiation therapy, or other medical conditions, can engulf the penis (StatPearls – Genital Lymphedema).
- Complications from Circumcision: In rare cases, removing too much foreskin during circumcision can cause scarring that tethers the penis, pulling it back into the pubic fat (StatPearls – Circumcision Complications).
- Lichen Sclerosus: A chronic inflammatory skin condition that creates scarring on the foreskin. This scarring can lead to phimosis (a tight, unretractable foreskin), which can trap the penis and pull it inward (Mayo Clinic).
How a Congenital Buried Penis Occurs in Children
A congenital buried penis occurs in children when the ligaments that anchor the base of the penis to the pubic bone are weak or abnormal, allowing the penis to retract inward (StatPearls – Congenital Buried Penis).
This condition is present at birth and is typically caused by:
- Weak Ligaments: The ligaments are abnormal, allowing the penis to be “hypermobile” and retract into the prepubic fat.
- Abnormal Skin Attachments: The skin of the scrotum may be attached too high up on the penile shaft, creating a “webbed” effect (penoscrotal webbing) that hides the penis’s length.
What Are the Key Symptoms of a Buried Penis?
The key “symptoms of a buried penis” are primarily functional and psychological, including severe urinary problems, poor hygiene, recurrent skin infections, and significant emotional distress from the concealed anatomy (PMC – Impact on QoL).
Primary symptoms include:
- Urinary Problems: Inability to urinate while standing, a spraying or misdirected urine stream, and chronic dribbling that soaks clothing and irritates the skin.
- Hygiene Issues: Significant difficulty or inability to clean the glans and penile skin, leading to a buildup of smegma (a mix of dead skin cells and oils).
- Recurrent Infections: The moist, trapped environment under the fat pad is an ideal breeding ground for bacteria and fungi, leading to chronic skin inflammation (dermatitis), balanitis (inflammation of the glans), and fungal infections (Candida).
- Sexual Dysfunction: Difficulty or impossibility of penetrative intercourse, painful erections (if the skin is tethered), and significant low self-esteem, depression, or anxiety related to genital appearance.
How Do Doctors Diagnose a Buried Penis?
Doctors diagnose a buried penis with a simple physical exam by pressing down on the suprapubic fat pad to reveal a penis of normal length, which definitively distinguishes it from a micropenis.
During this physical exam, the doctor will apply firm pressure on the pubic fat at the base of the penis. In a patient with a buried penis, this action will extrude the shaft, revealing a penis of normal length that is simply hidden.
This simple test confirms the diagnosis and clearly differentiates a buried penis from a micropenis. A micropenis is a rare congenital condition where the penis is anatomically fully formed but is an anatomically small penis that measures less than 2.5 standard deviations below the mean for its age (StatPearls – Micropenis).
What Is the Treatment for a Buried Penis?
The “treatment for a buried penis” is highly effective and aims to “unbury” the penis, with options ranging from significant weight loss for mild cases to surgical reconstruction for more severe conditions.
How Non-Surgical Treatments Can Manage a Buried Penis
Non-surgical “treatment for a buried penis” is effective only in mild cases, with significant weight loss being the primary method to reduce the suprapubic fat pad.
- Weight Loss: In cases directly caused by obesity, significant weight loss (sometimes achieved via bariatric surgery (StatPearls – Bariatric Surgery)) can reduce the size of the suprapubic fat pad. This may resolve the issue entirely or make a future surgical correction more effective and safer.
- Topical Steroids: For cases where Lichen Sclerosus is a contributing factor, strong steroid creams can help reduce inflammation and loosen tight, scarred foreskin.
- Hygiene: Diligent daily cleaning and drying of the trapped skin can help manage infections and inflammation but will not cure the underlying anatomical problem of the buried penis.
What Surgical Treatments Are Used to Repair a Buried Penis?
Surgical “treatment for a buried penis” involves a combination of procedures, led by an escutcheonectomy (fat pad removal), to release the penis and secure it in its proper position (PMC – Surgical Management).
The primary procedure is often an escutcheonectomy (or panniculectomy), which involves surgically removing the large pad of fat (escutcheon) and excess skin (pannus) from the suprapubic area. This uncovers the base of the penis (PMC – Surgical Management).
Other procedures are often performed at the same time to ensure a stable, long-term result (PubMed – Surgical Outcomes):
- Release of Ligaments: The surgeon may need to detach the abnormal or tight ligaments that are pulling the penis inward.
- Skin Grafts: After the penis is “unburied” (a process called degloving), a split-thickness skin graft is often required to cover the newly exposed penile shaft (ScienceDirect – Skin Grafts). This graft is typically taken from the thigh or buttock.
- Scrotoplasty: This is a procedure to reshape the scrotum if excess scrotal skin or penoscrotal webbing contributes to the problem.
- Tacking Sutures: The surgeon will place strong, internal stitches to anchor the skin at the base of the penis to the underlying pubic bone, preventing the penis from retracting back into the fat pad.
Glossary of Clinical Terms
To ensure full clarity, this glossary defines the key clinical and scientific terms used throughout this guide on buried penis.
| Term | Definition |
|---|---|
| Buried Penis | A medical condition where a normal-sized penis is hidden by excess skin and/or fat from the abdomen, scrotum, or thighs. |
| Micropenis | A rare congenital condition where the penis is anatomically normal but measures more than 2.5 standard deviations below the average size for age. |
| Suprapubic Fat Pad | The layer of adipose tissue (fat) located over the pubic bone at the base of the penis. |
| Escutcheonectomy | A surgical procedure to remove the escutcheon, or the pad of fat and excess skin, from the suprapubic area. |
| Phimosis | A condition in uncircumcised males where the foreskin is too tight to be retracted back over the glans. |
| Lichen Sclerosus | A chronic, inflammatory skin condition that can cause scarring and tightening of the skin, sometimes leading to phimosis. |