What Is Bowen Disease of the Penis? A Guide to Causes, Symptoms, and Treatment
Bowen disease of the penis is a precancerous skin condition that is a very early, noninvasive form of squamous cell carcinoma, also known as “squamous cell carcinoma in situ,” which is highly treatable when diagnosed early (DermNet NZ).
This condition, a type of penile intraepithelial neoplasia (PIN), involves abnormal cells, but they are confined entirely to the epidermis (the outermost layer of the skin) and have not invaded deeper tissues. Understanding this condition is the first step toward effective management.
This guide provides a clear, step-by-step framework to understand what Bowen disease of the penis is, its common causes, how to identify its symptoms, and the most effective treatment options. Because it is a form of carcinoma in situ, Bowen disease of the penis is not yet cancer, but it has the potential to become an invasive cancer if left untreated.
Key Takeaways on Bowen Disease of the Penis
- What it is: Bowen disease of the penis is a form of penile intraepithelial neoplasia (PIN), meaning it involves abnormal, precancerous cells confined to the outermost layer of the skin (epidermis) on the penis shaft or scrotum.
- Primary Cause: The main cause of Bowen disease of the penis is infection with high-risk strains of the human papillomavirus (HPV), most commonly HPV 16.
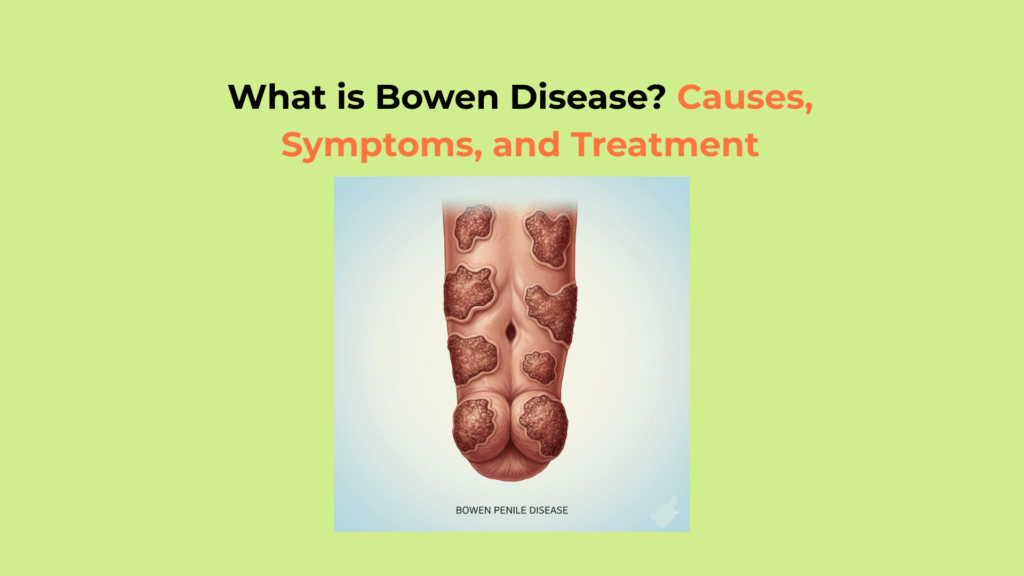
- Core Symptoms: The key symptom is a slow-growing, persistent, flat or slightly raised patch of skin. This patch is often reddish-brown, scaly, or crusty.
- Treatment Goal: Treatment for Bowen disease of the penis focuses on completely removing or destroying the abnormal cells to prevent them from progressing into an invasive squamous cell carcinoma.
What Causes Bowen Disease of the Penis?
The primary cause of Bowen disease of the penis is a persistent, long-term infection with high-risk strains of the human papillomavirus (HPV), the same virus responsible for most cervical and anal cancers (National Cancer Institute).
How HPV Infection Causes Bowen Disease of the Penis
HPV infection causes Bowen disease of the penis when its viral oncoproteins, E6 and E7, inactivate the body’s natural tumor-suppressing proteins (p53 and Rb), allowing skin cells to grow uncontrollably and become abnormal.
The vast majority of penile intraepithelial neoplasia (PIN) cases, including Bowen disease, are directly linked to these high-risk HPV infections (PMC – HPV-Associated Penile Lesions). The most common strain involved is HPV 16, followed by HPV 18. When the E6 and E7 proteins disrupt the normal cell cycle, the skin cells in the epidermis begin to replicate with abnormalities, leading to the precancerous lesion characteristic of Bowen disease of the penis.
What Are the Other Risk Factors for Bowen Disease of the Penis?
Other risk factors for Bowen disease of the penis include conditions that weaken the body’s ability to fight the HPV infection, such as immunosuppression, chronic smoking, or chronic inflammation. While HPV is the dominant cause, these factors can increase the likelihood of an infection persisting and developing into a lesion.
- Immunosuppression: A weakened immune system, whether from HIV or from medications taken for an organ transplant, makes it much harder for the body to clear the HPV infection on its own (CDC – Risk Factors).
- Chronic Smoking: Tobacco use is a well-established co-factor. The chemicals in smoke can damage DNA and further promote the progression of HPV-related lesions.
- Chronic Inflammation: A history of other inflammatory skin conditions on the penis, such as lichen sclerosus or chronic balanitis, may increase the risk of developing Bowen disease of the penis.
- Sun Exposure: It is important to note that while HPV is the main cause for genital lesions, chronic sun exposure is a primary cause for Bowen disease on other, non-genital parts of the body.
What Are the Key Symptoms of Bowen Disease of the Penis?
The key symptom of Bowen disease of the penis is a single, persistent, slow-growing, flat or slightly raised patch of skin (a plaque) that is often reddish-brown, scaly, or crusty.
Recognizing the Physical Appearance of Bowen Disease of the Penis
The physical appearance of Bowen disease of the penis is a distinct, well-defined skin lesion located on the penile shaft or scrotum. Unlike a temporary rash, this patch will persist and may slowly enlarge over months or even years.
- A single, persistent patch (plaque) on the skin of the penile shaft or scrotum (the hair-bearing areas).
- The patch is typically flat (macular) or only slightly raised (papular).
- It is often reddish, pink, or brownish in color.
- The surface may be scaly, crusty, or dry (hyperkeratotic).
- The lesion is usually slow-growing, over months or years, and has a clear, defined border.
How Bowen Disease of the Penis Differs from Similar Conditions
Bowen disease of the penis must be differentiated from two similar HPV-related conditions: Erythroplasia of Queyrat (which is on the glans) and Bowenoid Papulosis (which involves multiple small bumps). All are forms of penile intraepithelial neoplasia, but they appear in different locations and have different clinical features. This distinction is crucial for diagnosis (StatPearls – PIN).
| Condition | Typical Location | Typical Appearance | Key Differentiator |
|---|---|---|---|
| Bowen Disease (Penile) | Penile shaft, scrotum | Single, reddish-brown, scaly plaque | Histologically (under a microscope) it is a carcinoma in situ on hair-bearing skin. |
| Erythroplasia of Queyrat | Glans (head) or foreskin | Single, velvety, bright red, shiny plaque | This is just Bowen disease located on the non-hair-bearing mucosal skin (the glans or inner foreskin). |
| Bowenoid Papulosis | Genital/anal area | Multiple, small, pink or brown papules (bumps) | Often affects younger, sexually active adults and has a higher chance of regressing on its own, though it is also caused by HPV. |
How Do Doctors Diagnose Bowen Disease of the Penis?
Doctors diagnose Bowen disease of the penis definitively using a skin biopsy, which involves taking a small sample of the lesion for histopathology (microscopic examination) to confirm the presence of precancerous cells.
- Physical Examination: A dermatologist or urologist will first examine the lesion’s size, shape, color, and texture, noting its location on the shaft or scrotum.
- Dermoscopy: The doctor may use a special magnifying lens, called a dermoscope, to look for specific structural patterns within the lesion that can suggest a precancerous condition.
- Skin Biopsy: This is the only way to confirm a diagnosis. After applying a local anesthetic, the doctor removes a small sample of the lesion (a punch or shave biopsy) and sends it to a laboratory.
- Histopathology: This is the clinical term for the laboratory analysis (StatPearls – Histopathology). A pathologist performs histopathology by examining the tissue under a microscope to look for the characteristic full-thickness abnormal cells in the epidermis. This examination confirms that the condition is “in situ” (noninvasive).
What Is the Treatment for Bowen Disease of the Penis?
The “treatment for Bowen disease of the penis” is focused on the complete removal or destruction of the abnormal, precancerous cells, with options ranging from surgical excision to non-surgical topical creams and therapies (American Cancer Society). The goal is to eliminate the lesion before it has a chance to progress.
How Surgical Treatments Remove Bowen Disease of the Penis
Surgical treatments, such as standard surgical excision or Mohs surgery, are the most common and effective “treatments for Bowen disease of the penis,” offering high cure rates by physically removing the entire lesion.
- Surgical Excision: This is the most common treatment. The surgeon cuts out the entire lesion along with a small margin of healthy skin to ensure all abnormal cells are gone.
- Mohs Surgery: This is a specialized surgical technique often used in sensitive areas like the genitals (Skin Cancer Foundation). The doctor removes the lesion one thin layer at a time, checking each layer under a microscope during the procedure until no abnormal cells remain. This method preserves the maximum amount of healthy tissue.
How Non-Surgical Treatments Manage Bowen Disease of the Penis
Non-surgical “treatments for Bowen disease of the penis,” such as topical creams like Imiquimod or 5-Fluorouracil, are often used for larger lesions or when surgery is not ideal. These less invasive options can also be highly effective (American Cancer Society).
- Topical Creams: Creams like Imiquimod (which boosts the body’s own immune system to fight the virus and abnormal cells) or 5-Fluorouracil (a topical chemotherapy) are applied at home for several weeks.
- Cryotherapy: This method involves using liquid nitrogen to freeze and destroy the abnormal cells.
- Laser Ablation: A CO2 laser can be used to vaporize and destroy the lesion layer by layer.
- Photodynamic Therapy (PDT): A special light-sensitive cream is applied to the lesion. A few hours later, a specific wavelength of light is shined on the area, activating the cream and destroying the targeted cells.
What Is the Prognosis for Bowen Disease of the Penis?
The prognosis for Bowen disease of the penis is excellent when treated, as removal is typically curative; however, untreated lesions have a significant risk (up to 10%) of progressing to invasive squamous cell carcinoma (StatPearls – Bowen Disease).
Because the condition is “in situ,” the abnormal cells are contained within the top layer of skin and have not spread. Complete removal or destruction of the lesion effectively cures it (Cancer Research UK).
The primary danger of Bowen disease of the penis lies in ignoring it. Authoritative sources estimate that up to 10% of untreated genital Bowen disease cases can progress to become an invasive squamous cell carcinoma, which is a true skin cancer that can spread to other parts of the body. This is why medical evaluation is so critical.
The key to a positive outcome is prompt diagnosis and treatment. Do not ignore a persistent or changing skin lesion on the penis.