What Is Balanoposthitis? A Guide to Causes, Symptoms, and Treatment
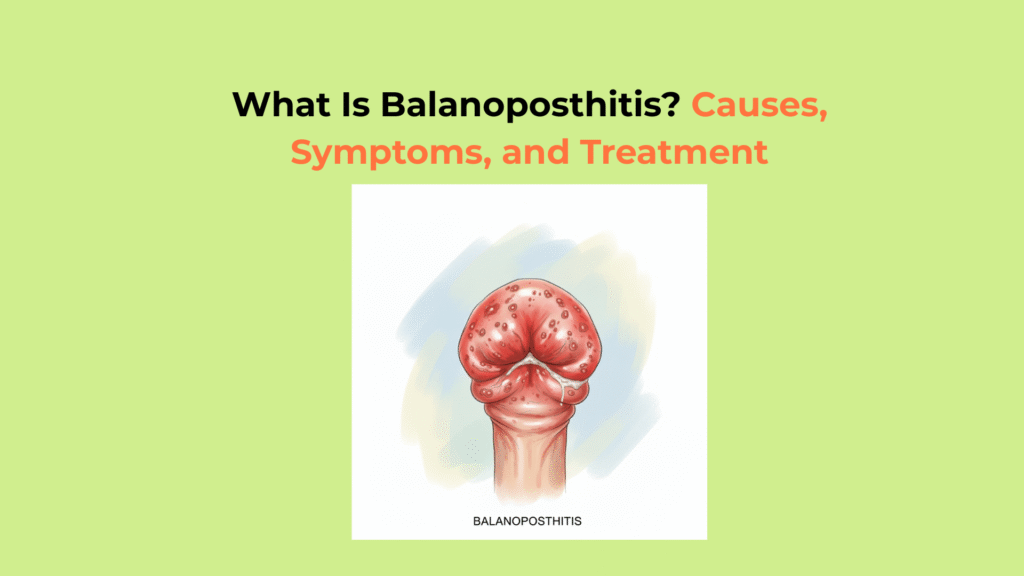
Balanoposthitis is the medical term for the simultaneous inflammation of the glans (head of the penis) and the foreskin (prepuce), a condition that only affects uncircumcised males (Cleveland Clinic) and causes pain, redness, and swelling.
While the symptoms are alarming, balanoposthitis is a common condition that is usually not serious and is easily treatable once the cause is identified. This guide provides a clear, evidence-based framework to understand what balanoposthitis is, its common causes, how to identify its symptoms, and the most effective treatment options.
Key Takeaways on Balanoposthitis
- What it is: Balanoposthitis is the simultaneous inflammation of the penis head (glans) and the foreskin (prepuce).
- Common Causes: The primary causes of balanoposthitis are poor hygiene and infections, most commonly a fungal (Candida) infection.
- Core Symptoms: Key symptoms include redness, swelling, itching, and a foul-smelling discharge from under the foreskin.
- Treatment Focus: Treatment for balanoposthitis targets the underlying cause, using antifungal creams, antibiotics, or hygiene improvements.
What Causes Balanoposthitis?
The primary causes of balanoposthitis are poor hygiene and infections, most commonly a fungal (Candida) infection (StatPearls – NCBI Bookshelf). Poor hygiene is often the key enabling factor, as it creates a warm, moist, and dark environment under the foreskin where pathogens can thrive.
This allows for the buildup of smegma, which is a natural, cheese-like substance made of exfoliated dead skin cells and oils. When not cleaned away, smegma can act as a breeding ground for bacteria and fungi, leading to inflammation.
How Infectious Agents Cause Balanoposthitis
Infectious agents, particularly the fungus Candida albicans, are the most common causes of balanoposthitis (Medscape), as they thrive in the warm, moist environment under the foreskin.
- Fungal Infections (Most Common): Typically caused by overgrowth of Candida albicans, the same yeast that causes thrush.
- Bacterial Infections: Common bacteria like Streptococcus or Staphylococcus can cause bacterial balanoposthitis.
- Sexually Transmitted Infections (STIs): Less commonly, herpes, gonorrhea, or syphilis can present with symptoms of balanoposthitis.
How Non-Infectious Factors Cause Balanoposthitis
Non-infectious “causes of balanoposthitis” include factors that directly irritate the skin, such as harsh soaps, or underlying health conditions like uncontrolled diabetes that promote infection.
- Irritants & Allergens: Chemical irritants found in harsh soaps, laundry detergents, lubricants, or latex condoms can cause an allergic reaction or direct skin irritation.
- Underlying Skin Conditions: Pre-existing conditions like eczema or psoriasis that affect the genital area can trigger inflammation.
- Uncontrolled Diabetes: This is a major risk factor. High blood sugar (hyperglycemia) can lead to glucose in the urine (glycosuria). This glucose-rich urine provides a perfect food source for yeast (Candida) to overgrow under the foreskin. (Cleveland Clinic).
What Are the Key Symptoms of Balanoposthitis?
The key symptoms of balanoposthitis include redness, swelling, itching, and a foul-smelling discharge from under the foreskin (Cleveland Clinic).
Recognizing Common Balanoposthitis Symptoms
Common “balanoposthitis symptoms” are all related to acute inflammation of the head of the penis and the foreskin.
- Redness, soreness, and swelling of the penis head and foreskin.
- Itching or a burning sensation in the affected area.
- A thick, white, or foul-smelling discharge (smegma) under the foreskin.
- Pain or discomfort during urination.
Identifying Severe Balanoposthitis Symptoms
Severe balanoposthitis symptoms require urgent medical attention, such as the inability to move the foreskin (phimosis) or the foreskin becoming trapped (paraphimosis).
- Phimosis: The inability to retract the foreskin due to swelling.
- Paraphimosis: The foreskin gets stuck in the retracted position, cutting off blood flow to the glans.
- Sores or ulcers on the glans.
- Painful, swollen lymph nodes in the groin.
Paraphimosis is a urologic emergency that cuts off blood flow to the glans (Mayo Clinic).
How Do Doctors Diagnose Balanoposthitis?
Doctors diagnose balanoposthitis through a physical exam and swab testing for bacteria, fungi, or viruses (Merck Manual). Blood and urine tests may be ordered for recurrent cases to check for diabetes.
- Physical Examination: A doctor will visually inspect the glans and foreskin for redness, discharge, and swelling.
- Medical History: The doctor will ask about hygiene habits, sexual activity, and underlying conditions like diabetes.
- Swab Test: A small sample of the discharge may be taken from under the foreskin to test for bacteria, fungi (Candida), or viruses.
- Blood & Urine Tests: If balanoposthitis is recurrent, these tests may be ordered to check for underlying, undiagnosed diabetes.
How Is Balanoposthitis Treated?
Treatment for balanoposthitis targets its underlying cause, using antifungal creams, antibiotics, or hygiene improvements (NHS).
How to Treat Fungal (Yeast) Balanoposthitis
Fungal (Yeast) Balanoposthitis: Treated with topical antifungal creams such as clotrimazole or miconazole (NHS).
How to Treat Bacterial Balanoposthitis
Bacterial Balanoposthitis: Treated with topical antibiotic creams (e.g., mupirocin) or oral antibiotics in severe cases.
How to Treat Irritant-Based Balanoposthitis
Irritant-Based Balanoposthitis: Managed by discontinuing the irritant and using mild steroid creams like hydrocortisone.
How At-Home Care Supports Balanoposthitis Treatment
At-home care for balanoposthitis supports medical treatment by reducing irritation and keeping the area clean and dry.
- Gently cleaning the area daily with warm water (no soap) and drying it thoroughly.
- Using warm salt baths to soothe irritation.
- Avoiding sexual contact until the inflammation has resolved.
How to Treat Recurrent or Chronic Balanoposthitis
Treating chronic or recurrent balanoposthitis requires managing the underlying cause, such as controlling blood sugar in diabetes, or considering circumcision as a permanent solution. This first involves a thorough medical evaluation to identify and manage conditions like diabetes or to test for less common infections.
For chronic or recurrent cases—especially those linked to phimosis—circumcision is a highly effective long-term solution (HealthDirect Australia).
Comparing Common Balanoposthitis Topical Treatments
This table compares the primary topical “treatments for balanoposthitis,” their target cause, and their mechanism of action.
| Treatment Type | Target Cause | Example | Action |
|---|---|---|---|
| Antifungal Cream | Yeast (Candida) | Clotrimazole | Kills the fungal infection. |
| Antibiotic Cream | Bacteria | Mupirocin | Kills the bacterial infection. |
| Steroid Cream | Irritation / Allergy | Hydrocortisone 1% | Reduces inflammation and itching. |
How Can Balanoposthitis Be Prevented?
Balanoposthitis can be prevented with good hygiene, managing underlying conditions like diabetes, and avoiding irritants. Always use condoms to prevent sexually transmitted infections that can cause balanoposthitis (CDC).
Balanoposthitis Prevention Checklist
When to See a Doctor for Balanoposthitis
You must see a doctor for balanoposthitis if symptoms do not improve within 2-3 days of good hygiene, if symptoms are severe (like sores or phimosis), or if you experience a medical emergency like paraphimosis.
A proper diagnosis is crucial for getting the correct treatment (e.g., an antifungal for a fungal infection, not an antibiotic). At [Your Clinic/Brand], we are committed to providing clear, factual health information to help you manage your health with confidence. Understanding that balanoposthitis is a common, treatable condition is the first step toward resolving it quickly.
Glossary of Clinical Terms
To ensure full clarity, this glossary defines the key clinical and scientific terms used throughout this guide on balanoposthitis.
| Term | Definition |
|---|---|
| Balanitis | Inflammation, redness, and swelling of the glans (head of the penis) only. |
| Balanoposthitis | Inflammation that involves both the glans (head of the penis) and the foreskin. |
| Glans | The sensitive, cone-shaped head or tip of the penis. |
| Smegma | A natural, cheese-like substance made of dead skin cells and oils that can build up under the foreskin. |
| Candida albicans | A type of yeast (fungus) that is the most common infectious cause of balanoposthitis. |
| Phimosis | A condition in uncircumcised males where the foreskin is too tight to be retracted back over the glans. |
| Paraphimosis | A urologic emergency where the retracted foreskin becomes trapped behind the glans, cutting off blood flow. |
3 Responses